Gut:浙江大学医学院徐骁教授团队Gut发表肝癌干性研究新成果
2019-12-07 佚名 细胞
<div>近日,国际著名<a class="channel_keylink" href="http://ipsen2017.medsci.cn/ipsen/sporty/show-details/3074/2" target="_blank"><a class="channel_keylink" href="http://ipsen2017.medsci.cn/ipsen/sporty/show-details/69/2" target="_blank">消化</a></a>杂志Gut在线发表了浙江大学医学院徐骁教授团队的题为USP22 promotes hypoxia-induced hepatocellular carcinoma stemness by a HIF1α/USP22 positive feedback loop upon TP53 inactivation的研究论文。</div><div><br>肿瘤组织中某些细胞亚群的<a class="channel_keylink" href="http://www.medsci.cn/article/list.do?q=%E
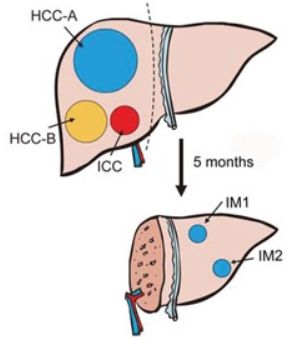
肿瘤组织中某些细胞亚群的干细胞特性被认为与肿瘤的发生、侵袭转移、血管新生和放化疗抵抗密切相关, 靶向肿瘤干细胞特性已成为克服肿瘤细胞耐药、抑制肿瘤转移与复发的重要策略。该研究发现,去泛素化蛋白酶 ubiquitin-specific protease 22(USP22) 可在缺氧条件下稳定肝癌细胞中的HIF1α蛋白;而在TP53失活的肝癌细胞中,HIF1α可促进USP22的转录表达。USP22与HIF1α组成的正反馈调节通路可促进肝癌细胞的干性表型。分析肝癌病人的组织标本发现,TP53失活突变合并USP22和HIF1α高表达的患者预后更差。TP53失活突变是肝癌发生发展中的常见事件,与肝癌的恶性生物学行为密切相关。该研究解析了USP22/HIF1α调控环路在TP53失活突变肝癌中的关键作用,揭示了维持肝癌干性的全新分子通路。
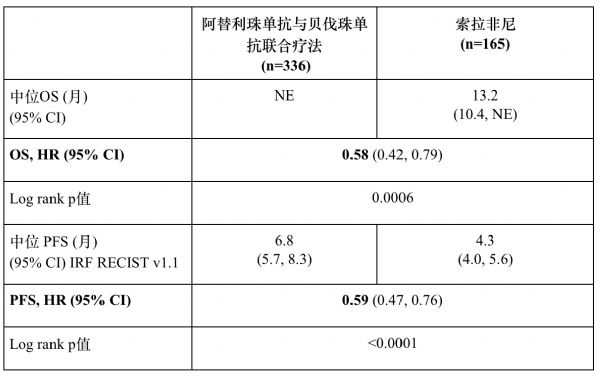
另外,鉴于目前缺少USP22的特异性抑制剂,该团队开发了一种新型肿瘤内活性氧响应的纳米基因药物,特异性降低肿瘤内USP22的表达,可显着抑制肝癌肿瘤的生长,并且增强肝癌细胞对索拉菲尼的敏感性,为肝癌的精准靶向治疗提供了有效的策略。
该论文通讯作者为***、浙江大学医学院附属第一医院肝胆胰外科徐骁教授。浙江大学医学院附属第一医院肝胆胰外科医师凌孙彬博士、博士生单巧楠、硕士生詹启帆为论文第一作者。该项研究受教育部***奖励计划、国家科技重大专项及国家杰出青年科学基金等项目资助,得到浙大一院领导和相关科室的支持。郑树森院士、申有青教授及美国宾夕法尼亚大学医学院部分学者给予大力支持。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#医学院#
37
#浙江大学#
42
#新成果#
34
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
59