AACR19:晚期三阴性乳腺癌患者经Ipatasertib与Tecentriq联合化疗的ORR高达73%
2019-04-02 不详 网络
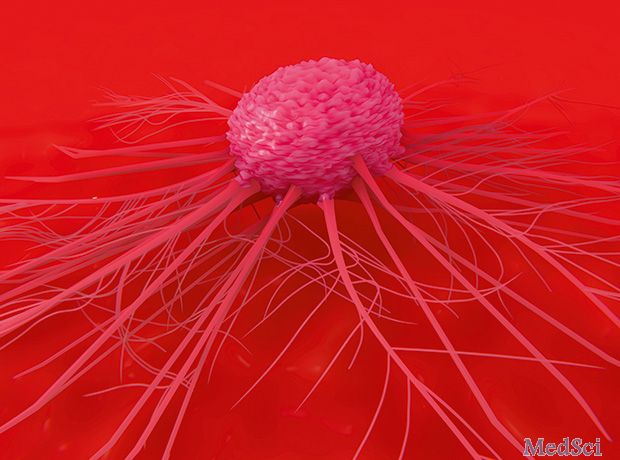
罗氏制药近日公布了一项Ib期研究的初步结果,该研究评估了Ipatasertib与Tecentriq(atezolizumab)联合治疗作为晚期三阴性乳腺癌(TNBC)患者的一线治疗方案的有效性。根据美国癌症研究协会(AACR)年会详述的结果,该方案证实了联合治疗方案的客观反应率(ORR)为73%,且与肿瘤生物标志物状态无关。
罗氏制药近日公布了一项Ib期研究的初步结果,该研究评估了Ipatasertib与Tecentriq(atezolizumab)联合治疗作为晚期三阴性乳腺癌(TNBC)患者的一线治疗方案的有效性。根据美国癌症研究协会(AACR)年会详述的结果,该方案证实了联合治疗方案的客观反应率(ORR)为73%,且与肿瘤生物标志物状态无关。
三阴性乳腺癌是指癌组织免疫组织化学检查:雌激素受体(ER)、孕激素受体(PR)和原癌基因Her-2均为阴性的乳腺癌。这类乳腺癌占所有乳腺癌病理类型的10.0%~20.8%,具有特殊的生物学行为和临床病理特征,预后较其他类型差。罗氏表示,无论PD-L1状态或PIK3CA状态如何,患者均可在Ipatasertib与Tecentriq联合化疗中获得反应。
原始出处:
http://www.firstwordpharma.com/node/1632490#axzz5jptFWRuj
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#晚期三阴性乳腺癌#
36
#TEC#
40
#阴性乳腺癌#
23
#ACR#
32
#联合化疗#
30
#三阴性#
29
#ATA#
23
#Tecentriq#
27
#AACR#
29
#乳腺癌患者#
25