NEJM:降低急性低氧性呼吸衰竭患者Pao2治疗目标对患者死亡风险的影响
2021-04-09 MedSci原创 MedSci原创
在ICU接受治疗的急性低氧性呼吸衰竭患者,将目标动脉氧分压从90mmHg降低至60mmHg不能降低患者死亡风险。
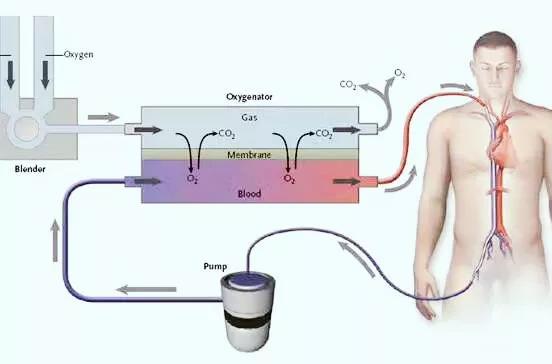
接受ICU治疗的急性低氧性呼吸衰竭患者往往需接受高浓度吸氧治疗以提高动脉氧分压(Pao2)。有学者认为,过高的动脉氧分压可导致患者死亡风险增加,有小规模研究发现,相比于周围血氧饱和度为96%以上的患者,目标Pao2在88%-92%可能对患者更有益;同时研究发现,目标Pao2在70-100mgHg患者的死亡率低于Pao2目标在150mmHg患者。

近日研究人员考察了动脉氧分压治疗目标对急性低氧性呼吸衰竭患者死亡风险的影响。
2928名因急性低氧性呼吸衰竭接受ICU监护的患者参与,所有患者均接受吸氧治疗,目标Pao2 为60 mm Hg(低氧分压组)或90 mm Hg(高氧分压组),随访90天。研究的主要终点是90天内死亡风险。
90天时,低氧分压组1441例患者中有618例(42.9%)死亡,而高氧分压组1447例患者中有613例(42.4%)死亡(校正风险比1.02)。在90天时,组间患者在无生命支持条件下存活天数或出院后存活天数百分比无显著差异。组间新发休克、心肌缺血、缺血性脑卒中或肠缺血风险相似。

研究认为,在ICU接受治疗的急性低氧性呼吸衰竭患者,将目标动脉氧分压从90mmHg降低至60mmHg不能降低患者死亡风险。
原始出处:
Olav L. Schjorring et al. Lower or Higher Oxygenation Targets for Acute Hypoxemic Respiratory Failure. N Engl J Med, April 8, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











好的
60
#患者死亡#
25
#死亡风险#
35
#PaO2#
30
#急性低氧性呼吸衰竭#
51
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
54
学习了
72