European Radiology:肾移植后MR心脏结构和功能的时间依赖性变化
2022-07-24 shaosai MedSci原创
心脏磁共振(CMR)是评估心脏结构和功能的金标准。CMR T1 mapping指标已被用于研究心肌间质纤维化,并显示出与心肌活检结果的明显相关性。
 众所周知,心血管疾病(CVD)是终末期肾病(ESRD)患者的主要死因。作为ESRD患者的最佳治疗方法,肾脏移植(KT)与心血管死亡率的降低有关。然而,心血管疾病仍然是导致KT受体死亡的主要原因之一。肾移植受者的心血管疾病风险明显高于普通人群,KT后心血管相关死亡的最常见原因是心脏骤停和心律失常。心脏结构的异常,如心肌纤维化和左心室肥厚(LVH),是导致KT受体心血管风险增加的原因。因此,评估KT前和KT后心脏结构和功能的变化模式有助于进一步了解KT受体的心血管疾病的机制。
众所周知,心血管疾病(CVD)是终末期肾病(ESRD)患者的主要死因。作为ESRD患者的最佳治疗方法,肾脏移植(KT)与心血管死亡率的降低有关。然而,心血管疾病仍然是导致KT受体死亡的主要原因之一。肾移植受者的心血管疾病风险明显高于普通人群,KT后心血管相关死亡的最常见原因是心脏骤停和心律失常。心脏结构的异常,如心肌纤维化和左心室肥厚(LVH),是导致KT受体心血管风险增加的原因。因此,评估KT前和KT后心脏结构和功能的变化模式有助于进一步了解KT受体的心血管疾病的机制。
心脏磁共振(CMR)是评估心脏结构和功能的金标准。CMR T1 mapping指标已被用于研究心肌间质纤维化,并显示出与心肌活检结果的明显相关性。据报道,心肌变形对早期或细微的功能障碍更敏感。一些研究应用这些方法评估KT后心脏结构和功能的变化,然而这些研究均集中在单一时间点的变化,却不能反映KT后心脏变化的时间依赖性。
近日,发表在European Radiology杂志的一项研究利用多参数CMR探讨了KT前和KT后3、6和中位14个月的心脏结构和功能变化的时间依赖性,为该类患者的无创心功能评估提供了技术支持及数据参考。
本项回顾性研究分析了53名进行了KT前和KT后CMR检查的患者。根据KT后CMR的时间,将患者分为三组:第一组(KT后3个月,n = 16),第二组(KT后6个月,n = 21),第三组(KT后9个月以上,n = 16)。本研究同时招募了21名年龄和性别匹配的健康对照组(HC)。比较了CMR得出的左心室体积、左心室质量指数(LVMi)、左心室射血分数(LVEF)、整体径向应变(GRS)、整体周向应变(GCS)、整体纵向应变(GLS)和原始T1值。评估了CMR参数变化之间的关联。
第2组(p < 0.001)和第3组(p = 0.004)的KT后LVMi下降,但与HC相比,两组的LVMi值都较高(均p < 0.001)。KT后的GLS在第1组中减少(p = 0.021),但在第2组(p = 0.728)和第3组(p = 0.100)中略有增加,没有明显的差异。第3组的KT后GLS与HC没有区别(p = 0.104)。第2组和第3组KT后的LVEF、GRS和GCS明显增加,与HC无明显差异。所有三组的KT后原始T1值都明显下降;然而,没有一组与HC有任何明显差异。LVEF的变化与GCS、GRS和GLS的变化有关。
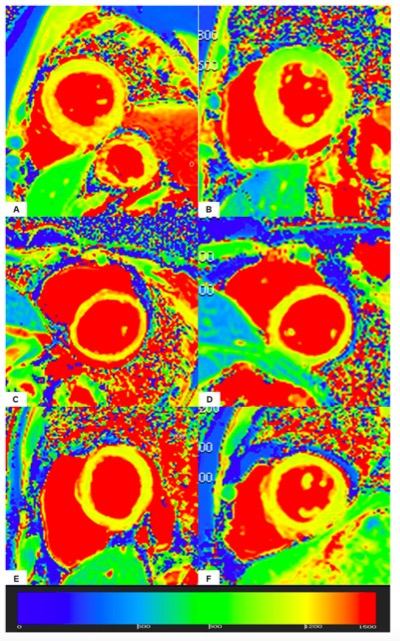 图 肾脏移植前后T1 maps的代表性示例。A和B组来自第1组的一位26岁患者的KT前和KT后的T1 maps。基线时,LVMi为109.24 g/m2,LVEF为59.69%,GRS为31.49%,GCS为-17.98%,GLS为-14.59%,原始T1值为1236.33 ms。KT后约3.40个月,LVMi为99.69g/m2,LVEF为65.59%,GRS为25.12%,GCS为-15.58%,GLS为-9.26%,原始T1值为1123.00ms。C和D是来自第2组的一名23岁患者的KT前和KT后的T1 maps。基线时,LVMi为46.23 g/m2,LVEF为42.81%,GRS为20.50%,GCS为-14.05%,GLS为-14.43%,原始T1值为1342.33 ms。KT后约7.07个月,LVMi为50.74g/m2,LVEF为66.70%,GRS为31.53%,GCS为-18.91%,GLS为-16.72%,原始T1值为1196.00ms。E和F是来自第3组的一名28岁的患者的KT前和KT后的T1 maps。基线时,LVMi为81.46 g/m2,LVEF为61.44%,GRS为27.71%,GCS为-17.13%,GLS为-14.51%,原始T1值为1198.33 ms。KT后约11.10个月,LVMi为61.94 g/m2,LVEF为74.12%,GRS为44.56%,GCS为-22.38%,GLS为-16.46%,原始T1值为1193.67 ms
图 肾脏移植前后T1 maps的代表性示例。A和B组来自第1组的一位26岁患者的KT前和KT后的T1 maps。基线时,LVMi为109.24 g/m2,LVEF为59.69%,GRS为31.49%,GCS为-17.98%,GLS为-14.59%,原始T1值为1236.33 ms。KT后约3.40个月,LVMi为99.69g/m2,LVEF为65.59%,GRS为25.12%,GCS为-15.58%,GLS为-9.26%,原始T1值为1123.00ms。C和D是来自第2组的一名23岁患者的KT前和KT后的T1 maps。基线时,LVMi为46.23 g/m2,LVEF为42.81%,GRS为20.50%,GCS为-14.05%,GLS为-14.43%,原始T1值为1342.33 ms。KT后约7.07个月,LVMi为50.74g/m2,LVEF为66.70%,GRS为31.53%,GCS为-18.91%,GLS为-16.72%,原始T1值为1196.00ms。E和F是来自第3组的一名28岁的患者的KT前和KT后的T1 maps。基线时,LVMi为81.46 g/m2,LVEF为61.44%,GRS为27.71%,GCS为-17.13%,GLS为-14.51%,原始T1值为1198.33 ms。KT后约11.10个月,LVMi为61.94 g/m2,LVEF为74.12%,GRS为44.56%,GCS为-22.38%,GLS为-16.46%,原始T1值为1193.67 ms
本研究表明,KT对心脏结构和功能有良好的影响。在KT后14个月的中位随访中,GRS、GCS、GLS和原始T1值逆转到正常水平,而LVMi却没有逆转,这有助于进一步解释为什么KT接受者的心血管风险仍在增加这一现象。
原文出处:
Li Qi,Xuefeng Ni,U Joseph Schoepf,et al.Time-dependent cardiac structural and functional changes after kidney transplantation: a multi-parametric cardiac magnetic resonance study.DOI:10.1007/s00330-022-08621-w
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#PE#
43
#肾移植后#
51
十五字十五字十五字十五字十五字
33
#心脏结构#
56