TCT 2018丨局麻是手术中高危患者行TAVR的良好选择
2018-09-27 国际循环编辑部 国际循环
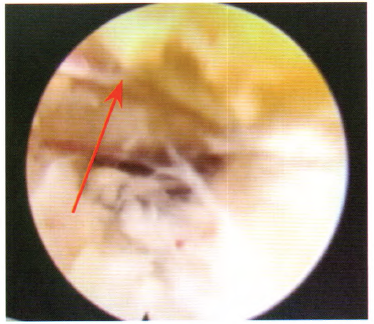
2018年9月23日,第30届TCT科学年会上发布的SOLVE-TAVI研究最新结果显示,手术中高危患者行经导管主动脉瓣置换术(TAVR)时采用局麻和全麻均同样安全有效;采用第一代球囊可扩张瓣膜与当前新一代自膨胀瓣膜的结局相似。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#局麻#
26
#AVR#
35
#高危患者#
29
#TCT#
28
好
66