JAMA Netw open:新生儿端粒长度与儿童血压的关系
2022-08-07 liangying MedSci原创
心血管健康可能在某种程度上在出生时就被规划,与TL密不可分。
成年人的心血管疾病往往源于生命早期的危险因素。在整个生命周期中,血压随着年龄的增长而显著升高。血压从儿童期到青春期和成年期都有变化,而高血压与晚年的心血管疾病有关。
端粒是覆盖染色体末端的核蛋白复合物,由于细胞分裂和年龄增长而缩短。端粒长度(TL)被认为是与成人心血管疾病(CVD)和死亡率相关的年龄生物学指标,端粒功能失调相关的血管壁衰老和内皮功能受损可以解释为什么在高血压患者中观察到TL缩短。有研究者推测出生时的TL可能包含晚年心血管健康和疾病的早期生物学信息。本研究的目的是评估新生儿TL是否与童年早期血压差异有关。
该队列研究是ENVIRONAGE(环境对早期衰老的影响)研究的一部分,是比利时母子对的出生队列研究,在2014年10月至2021期间进行出生时招募,中位随访4.5年。纳入分析的参与者提供了完整数据,以便在随访时进行评估。数据分析于2021年8月至9月进行。
应用定量聚合酶链反应(qPCR)检测新生儿脐带血和胎盘平均相对TL。随访时评估收缩压、舒张压和平均动脉压(MAP)。儿童高血压(根据儿童年龄、性别和身高进行标准化)的定义遵循2017年美国儿科学会指南。采用多变量调整线性和逻辑回归模型将新生儿TL与儿童时期血压指标联系起来。
该研究包括485名新生儿(52.8%为女孩),随访时平均年龄为4.6(0.4)岁。新生儿TL与儿童期低血压相关。脐带血TL的1-IQR增加与-1.54mmHg的舒张压降低和-1.18mmHg的MAP降低相关。未观察到与收缩压相关。此外,脐带血TL的1-IQR增加与4至6岁时患高血压的几率较低相关。在胎盘中,TL的1-IQR增加与舒张压降低-0.96mmHg、MAP降低-0.88mmHg和儿童期高血压的调整OR降低0.69相关。
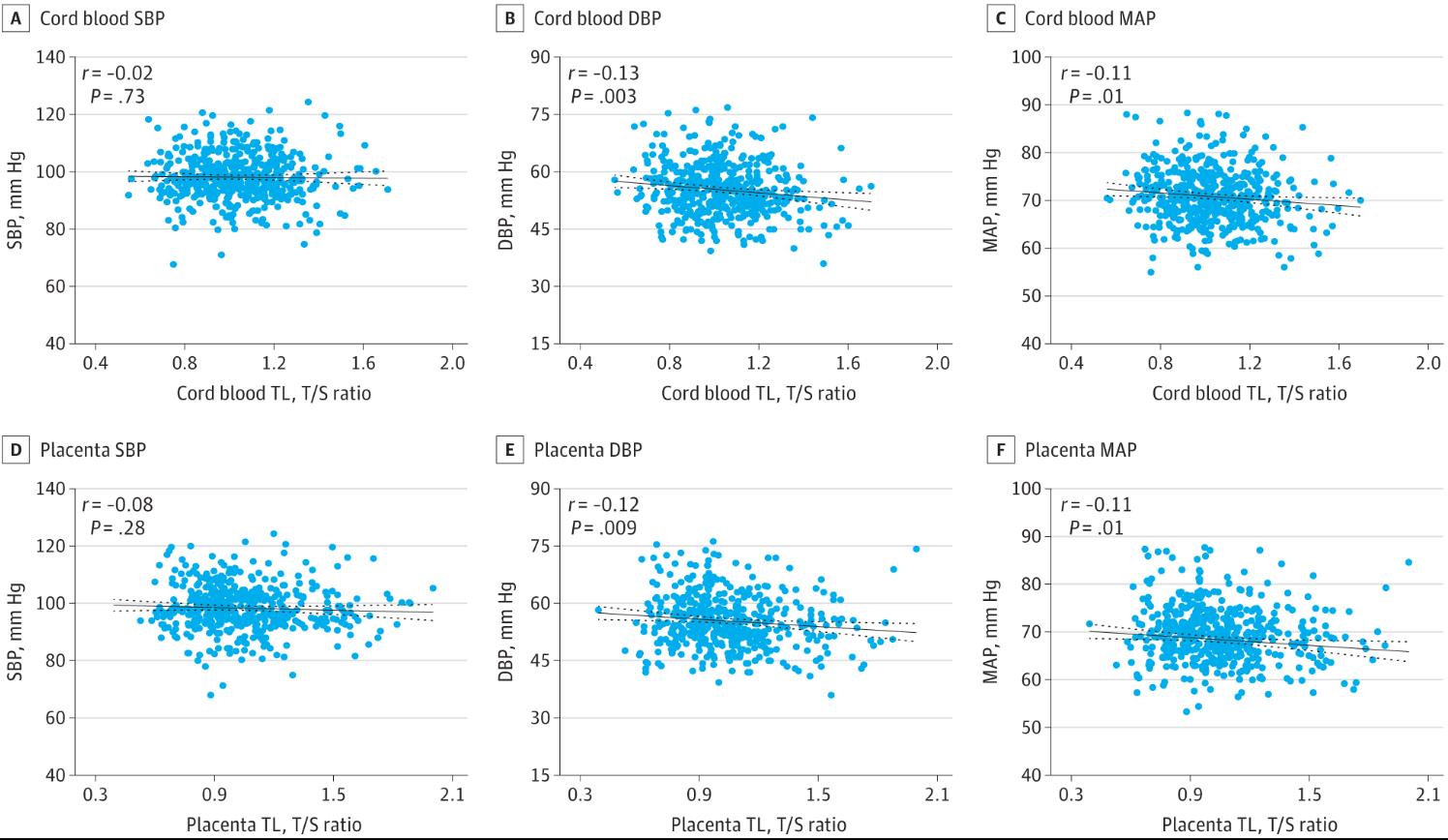
4- 6岁新生儿端粒长度(TL)与血压的Pearson相关性
总之,在这项前瞻性出生队列研究中,学龄早期血压变化与出生时TL相关。心血管健康可能在某种程度上在出生时就被规划,与TL密不可分。
参考文献:Martens DS, Sleurs H, Dockx Y, Rasking L, Plusquin M, Nawrot TS. Association of Newborn Telomere Length With Blood Pressure in Childhood. JAMA Netw Open. 2022;5(8):e2225521. doi:10.1001/jamanetworkopen.2022.25521
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#NET#
47
#PE#
22
#端粒长度#
46
JAMA上文章都是顶级的,谢谢梅斯及时上新
0