JAMA Surg:症状性胆结石患者术后疼痛症状缓解影响因素研究
2021-08-18 MedSci原创 MedSci原创
该模型可有效预测胆结石患者术后疼痛缓解的可能性,从而帮助外科医生决定胆结石患者是否能从胆囊切除术中获益。

在西方,胆结石的终生患病率为10%-20%,特别是肥胖人群的胆结石风险更高。在胆结石患者中,只有5%的患者存在相关并发症,如胆囊炎、胆管炎或胆汁性胰腺炎。胆囊切除术是最常见的胃肠道手术,但在临床实践中医生对胆囊结石疾病的治疗选择缺乏共识,胆囊切除术率在不同地区之间差异很大。近日研究人员开发了一种临床决策工具,针对不同症状的胆结石患者,预测手术对患者术后疼痛缓解的作用。
本次研究在荷兰25个医疗中心开展,包括1561名症状性单纯胆结石患者,临床定义为非复杂胆石症征象的胆结石患者,临床症状包括胆源性胰腺炎、胆管炎、胆总管结石或胆囊炎。收集患者基线检查和6个月随访时特征、共病、手术结果、疼痛和症状数据。研究的主要终点为术后无疼痛状态或与临床相关的疼痛减轻
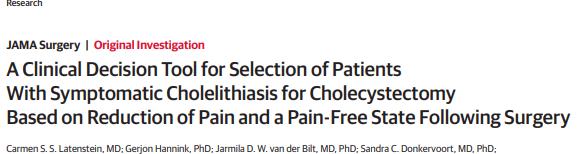
工具开发队列包含494名患者,验证队列包含1067名患者。在开发队列中,395名患者(80.0%)接受了胆囊切除术。手术后,225名患者(57.0%)报告无疼痛,295名患者(74.7%)报告了与临床相关的疼痛减轻。多变量预测模型显示,年龄增加、无腹部手术史、基线疼痛评分较高、背部放射疼痛、单纯止痛药止痛、恶心和无胃灼热是胆囊切除术后临床相关疼痛减轻的独立预测因素。验证队列中,预测工具具有较高的区分效果(C指数为0.80)。
患者症状、干预与预后
研究认为,该模型可有效预测胆结石患者术后疼痛缓解的可能性,从而帮助外科医生决定胆结石患者是否能从胆囊切除术中获益。
原始出处:
Carmen S. S. Latenstein et al. A Clinical Decision Tool for Selection of Patients With Symptomatic Cholelithiasis for Cholecystectomy Based on Reduction of Pain and a Pain-Free State Following Surgery. JAMA Surg. August 11,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











赞
82
#影响因素#
53
认真学习
83
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
81