Cell Metab:武大李红良课题组发现代谢风险成为缺血性心脏病的主要驱动因素
2021-09-03 haibei MedSci原创
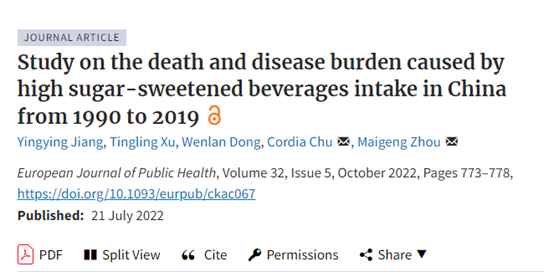
最近李红良课题组及其合作课题组利用2019年全球疾病负担研究(GBD)报告的数据,分析了1990年至2019年期间204个国家和地区的IHD死亡人数和年龄标准化死亡率(ASDRs)。
近几十年来,经济的快速发展和社会的进步大大增加了代谢性危险因素的发生率,其中包括高收缩压(SBP)、高低密度脂蛋白胆固醇(LDL-c)、高空腹血浆葡萄糖(FPG)和高体重指数(BMI)。这些风险因素在个人和人群层面对健康有着广泛而深远的影响。 在全球范围内,缺血性心脏病(IHD)与所有心血管疾病(CVDs)中最高的疾病负担有关,其中包括急性心肌梗死、慢性稳定型心绞痛、慢性IHD及其相关的心力衰竭。2019年,与IHD相关的死亡总数达到914万,占所有CVD相关死亡人数的49.2%。因此,随着时间的推移,代谢性危险因素对IHD死亡的影响值得调查。 武汉大学李红良课题组长期关注代谢性疾病及其对CVD的贡献,他们注意到,代谢性危险因素发生率的大幅增加阻碍了人们对各种CVD发病率和相关死亡率的控制,包括IHD在内。对于占世界人口80%以上的发展中国家来说,解决这一日益增长的预防和治疗需求变得尤为迫切,这些国家的疾病模式正在从以传染病为主转向以非传染性疾病(NCDs)为主。因此,对整体IHD负担、其流行病学特征以及任何相关的代谢、环境和行为风险因素的全面和最新的了解,对于公共卫生专家和政策制定者
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#CEL#
36
#驱动因素#
39
#Cell#
35
#MET#
28
#Meta#
27
#缺血性#
26
管理
65
#缺血性心脏病#
39