Clinical Infectious Disease: 高血压和使用钙通道阻滞剂对结核病治疗结果的影响
2021-11-08 MedSci原创 MedSci原创
结核病是由结核杆菌感染引起的慢性传染病。结核菌可能侵入人体全身各种器官,但主要侵犯肺脏,称为肺结核病。
结核病 (TB) 在世界范围内造成死亡的主要原因之一,2018 年约有150万人死于结核病,其中近90%的病例来自发展中国家,与此同时,许多低收入和中等收入国家的高血压患病率急剧上升,占全球高血压病例的近 75%。结核病和高血压高负担国家之间存在相当大的重叠。与没有结核病的对照组相比,结核病患者的高血压比例更高,多项队列研究表明,结核病后心血管和脑血管疾病的风险增加。高血压与全身炎症有关,包括白介素 (IL)-1、IL-18 和肿瘤坏死因子 (TNF)-α 水平升高。钙通道阻滞剂(CCB)是治疗高血压的一线药物。在临床前研究中,L 型电压门控钙通道的阻断已证明可改善分枝杆菌清除率。非二氢吡啶类 CCB(非DHP-CCB),如维拉帕米,可作为外排泵抑制剂,降低巨噬细胞中的细菌负荷并增加贝达喹啉对小鼠模型中结核分枝杆菌的杀菌活性。虽然钙通道阻滞剂 (CCB) 可改善临床前模型中的结核病治疗结果,但其对结核病患者的影响尚不清楚。因此,本项研究旨在对钙通道阻滞剂对结核病治疗结果的影响进行探究。

这项回顾性队列研究纳入了2000年至2016年在国立台湾大学医院接受敏感性结核病治疗的所有18岁以上患者,然后评估了高血压和CCB使用与在结核病治疗的前 9 个月,以及在第 2 个月和第 6 个月的痰涂片镜检和痰培养阳性的患者中全因和感染相关死亡率的关联。
在2894名患者中,1052 名 (36.4%) 患有高血压。多变量分析显示,高血压与全因死亡率([HR],1.57;95%[CI],1.23-1.99)和感染(HR,1.87;95% CI,1.34-2.6 )增加有关,但根据高血压组分层时,微生物学结果没有统计学差异。通过单变量 Cox 回归,使用二氢吡啶-CCB (DHP-CCB) 仅与降低全因死亡率(HR,0.67;95% CI,0.45–.98)相关。在单变量或多变量回归分析中,DHP-CCB 的使用与感染相关死亡率(HR,0.78;95% CI,0.46-1.34)或微生物结果之间没有关联。
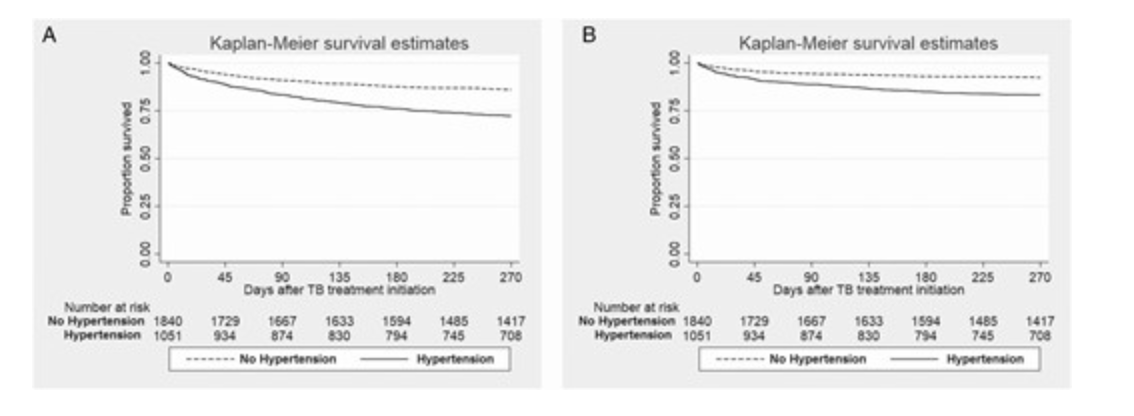
本项研究发现在开始结核病治疗后的9个月内,高血压患者的全因死亡率和感染相关死亡率均有所增加。DHP-CCB 的使用可能会降低高血压结核病患者的全因死亡率。高血压的存在或CCB的使用不会导致结核疾病病情的显着变化。
原始出处:
Vignesh Chidambaram. Et al. The Impact of Hypertension and Use of Calcium Channel Blockers on Tuberculosis Treatment Outcomes. Clinical Infectious Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Dis#
67
#阻滞剂#
52
#结核#
55
#clinical#
57
#治疗结果#
73