JMRI:高血压和脑血管病变的并存与WMH的存在有关
2021-11-05 MedSci原创 MedSci原创
血压引起的脑血管结构改变与WMH有关。提示血压升高可能是脑血管病变与小血管病变并存的病理生理机制之一。
脑白质高信号病灶被认为是阿尔兹海默症的核心改变,会加速阿尔茨海默病痴呆症相关区域的大脑萎缩模式。在血管危险因素中,慢性高血压是导致WMH的脑血管病理最重要的危险因素之一。有研究表明,从成年早期到中年,血压升高与WMH体积的增加有关。从病理变化的角度来看,高血压患者的白质病变通常是大脑的小动脉、小动脉和毛细血管出现了硬化 、坏死。
研究发现高血压与脑动脉病变的有关,包括小动脉的稀疏和大动脉的硬化。并且提出小血管病变可能与大血管病变相关的假说。脑血管形态学改变和WMH之间的联系得到了在年轻人中的一项研究的支持,该研究表明WMH病变计数(WMHC)与脑血管密度有关。在老年人中,脑血管改变是否与WMH相关,以及WMH、高血压和脑血管之间是否存在内在联系仍需要进一步研究。MRA和T2 FLAIR图像的研究进展使脑血管形态的自动量化和小血管病变的分析成为可能。Xingdong Chen等利用多参数脑MRI来研究老年社区人群中脑血管形态、高血压和CSVD之间的关系。研究结果发表在JMRI杂志。
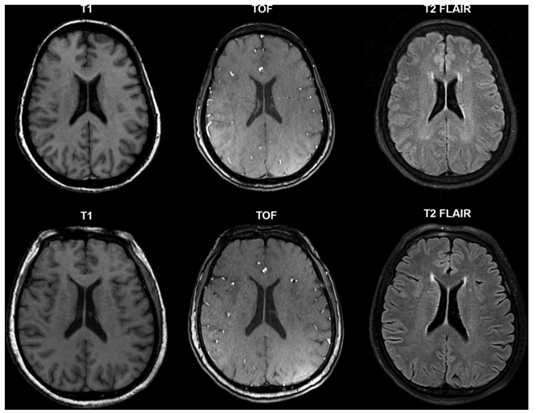
纳入863名(54.2%)无神经系统疾病临床证据的受试者分析。根据TOF MRA图像对脑血管形态学测量进行量化,包括血管密度、半径、弯曲程度和分支数量。根据T2 FLAIR图像自动计算WMH病灶体积(WMHV)和WMH病灶计数(WMHC)。
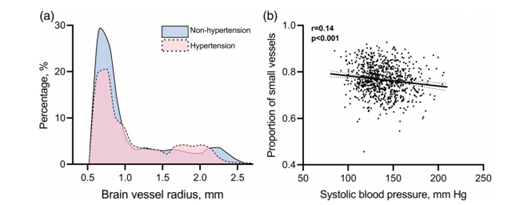
小血管比例随血压升高而降低。
高血压,尤其是舒张压与脑血管密度降低(β=-104)和分支数量减少(β=-0.02)显著相关。脑血管曲度降低(β=1.25)、半径增大(β=93.8)与血压呈正相关,但小血管曲度(β=-4.6 *10-4,P=0.58)和半径(β=0.03,P=0.0 8)与血压无显著相关。小血管比例随血压升高而减少(SBP:β=-6.6 *10-4;DBP:β=-9.0*10-4)。
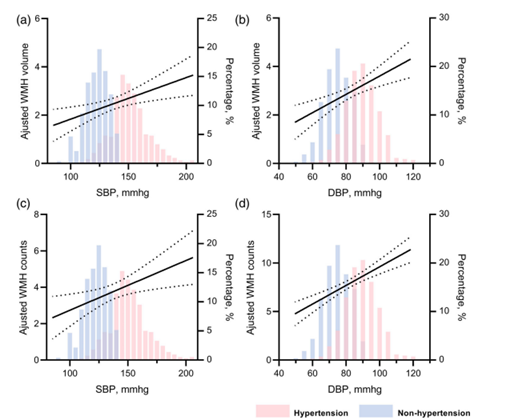
调整后白质高信号病变体积(WMHV)和白质高信号计数(WMHC)与收缩压(SBP)和舒张压(DBP)相关。
WMHV和WMHC增加与血管密度降低(体积:β=-2 4,计数:β=-127)、曲度降低(体积:β=-0.0 8,计数:β=-0.53)和半径增大(体积:β=12.6,计数:β=86.6)相关。路径分析表明,高血压和WMH之间存在关联,这种关联是由脑血管形态学变化介导的。
综上所述,高血压引起的脑血管结构改变与WMH有关。提示血压升高可能是脑血管病变与小血管病变并存的病理生理机制之一。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血管病#
51
#脑血管病变#
50
#WMH#
49
很有帮助
0
#血管病变#
43