Nat Commun:科学家发现阿尔茨海默病的潜在治疗靶点!
2022-04-23 生物谷 生物谷
该项研究表明,脑脂肪酸代谢将AD基因与下游免疫,突触和功能障碍联系起来,将SCD确定为AD治疗的潜在靶标。
阿尔茨海默病以家族性和散发性形式出现。家族性 AD 由改变淀粉样蛋白前体蛋白加工的常染色体显性突变引起。相反,虽然没有单一的散发性 AD 病因,但其发病率因与脂质代谢、免疫和突触功能相关的基因变异而增加。尽管具有独特的遗传基础,但家族和散发形式会出现类似的认知缺陷和几乎无法区分的神经病理学,包括淀粉样蛋白、tau、脂质、免疫和突触的异常。这些病理与其各自在AD发展中的作用之间的确切联系尚不清楚。其中,脂质异常是这些病理中调查和了解最少的。前期研究表明,SCD抑制剂(SCDi)输注到症状前AD小鼠的心室中减少了富含MUFA的甘油三酯的积累,并挽救了脑室周围和海马神经干细胞活性的早期下降。由于海马体是AD功能障碍的关键位点,那么SCDi是否可以改善海马功能呢?
近日,舍布鲁克大学的研究学者在Nat Commun上发表了一篇题为“Stearoyl-CoA Desaturase inhibition reverses immune, synaptic and cognitive impairments in an Alzheimer’s disease mouse model”的研究性论文,研究了硬脂酰辅酶A去饱和酶(SCD)在AD发病机制中的作用,SCD是脂肪酸去饱和度的关键调节剂。
AD14 的 3xTg 小鼠模型携带人类 APPSwe、tauP301L 和 PS1M146V 突变,早在6个月大时,在明显的淀粉样斑块和神经原纤维缠结发作之前,就会出现学习和记忆障碍症状。在本研究中,为了更好地了解早期有症状的3xTg海马体的遗传状态,他们对8个月大的雌性野生小鼠和3xTg小鼠进行了全海马RNA测序。结果表明,家族性AD的3xTg模型发展了脂质,免疫和突触基因的变化,这些生物学类别与散发性AD的发病机制有关;脂质代谢基因的转录组学变化是3xTg海马体的突出特征;MUFA代谢缺陷可能特别相关。
鉴于脂肪酸代谢基因(包括SCD)在症状阶段在海马体中明显失调,研究人员猜测SCD活性可有助于观察到的转录组学紊乱。经研究发现,脑室内施用SCDi1个月会深刻影响3xTg海马基因表达谱。SCD抑制在WT和3xTg小鼠之间恢复了超过40%的DEG。GO富集分析表明,SCD抑制可能正在影响与神经系统发育和突触相关的生物过程。此外,研究发现,SCD 抑制可逆转空间学习和记忆中的 3xTg 缺陷,而焦虑、神经干/祖细胞增殖、淀粉样蛋白负荷、tau高磷酸化和神经元损失保持不变。在3xTg小鼠中施用SCDi对海马突触相关基因表达产生广泛影响,并导致海马树突棘,树突状结构和活性相关IEG表达的恢复。通过单细胞分析,确定MHC-I基因是3xTg海马小胶质细胞中SCDi的主要靶标,此外,SCDi改变3xTg海马体中小胶质细胞的细胞景观。
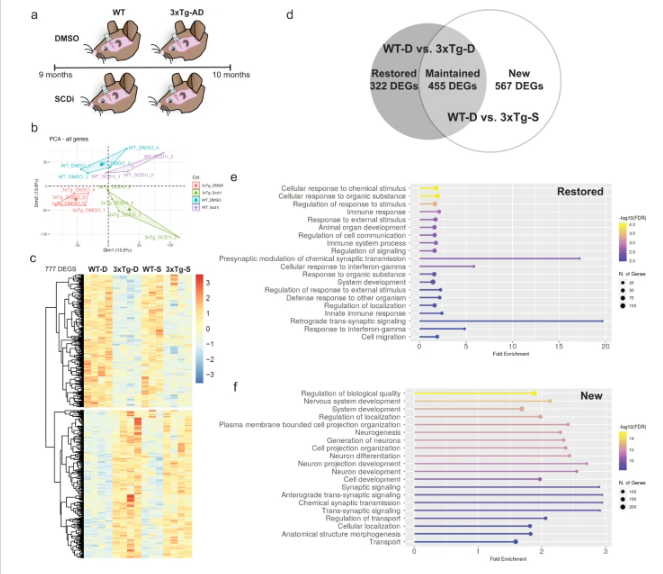
图 SCDi输注有效调节3xTg海马体中的基因表达,对免疫和突触相关基因有主要影响
总之,该项研究表明,脑脂肪酸代谢将AD基因与下游免疫,突触和功能障碍联系起来,将SCD确定为AD治疗的潜在靶标。
参考文献:
Hamilton, L.K., Moquin-Beaudry, G., Mangahas, C.L. et al. Stearoyl-CoA Desaturase inhibition reverses immune, synaptic and cognitive impairments in an Alzheimer’s disease mouse model. Nat Commun 13, 2061 (2022). https://doi.org/10.1038/s41467-022-29506-y
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#阿尔茨海#
34
#COMMUN#
0
#Nat#
28
#科学家发现#
42
#治疗靶点#
38
#阿尔茨#
31
#阿尔茨海默#
29