Nature子刊:新冠死亡率激增!免疫补体和凝血脱不了干系!补体抑制剂亟需开发!
2020-08-05 转化医学网 转化医学网
补体是一种血清蛋白质,活化后具有酶活性、可介导免疫应答和炎症反应。与补体相关的研究表明,现有的抑制补体系统的药物可以帮助治疗重症患者。
研究结果为了解COVID-19的病理生理学的提供了重要见解,并阐明了补体和凝血途径在确定SARS-CoV-2感染患者的临床结局中的作用。该研究发表在《自然医学》上。

补体在肥胖症和糖尿病中也更活跃,这可能至少部分解释了为什么患有这些疾病的人死于COVID的风险更大。有凝血功能障碍病史的人死于COVID感染的风险也增加了。
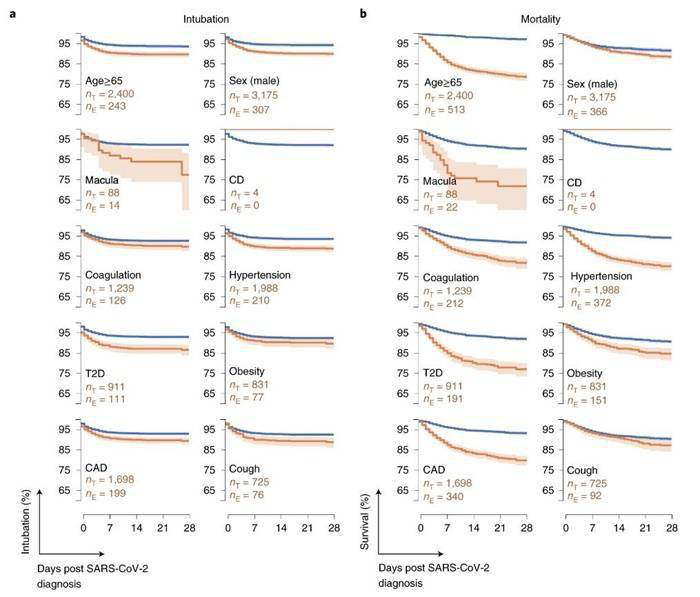

确定的SARS-CoV-2感染后,黄斑变性和凝血障碍的病史与不良预后相关
凝血和补体途径被激活
【1】https://medicalxpress.com/news/2020-08-ancient-immune-underpin-severe-covid-.html
【2】https://www.nature.com/articles/s41591-020-1021-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#激增#
31
#补体抑制剂#
36
#抑制剂#
37
#Nat#
41
新冠肺炎,疫情何时才能消失
55