J Clin Oncol:短程雄激素抑制和放疗剂量增加显著改善了中危前列腺癌患者的长期预后
2021-07-28 Nebula MedSci原创
6 个月的伴随和辅助 AS 治疗显著改善了接受 74 或 78 Gy 放射治疗的中危前列腺癌患者的 EFS 和 DFS
EORTC试验22991显示,6 个月的伴随和辅助雄激素抑制(AS)可提高接受外照射放疗(70-78 Gy)的中高风险的局部前列腺癌患者的生存预后(无进展生存期[EFS]和无病生存期[DFS])。
根据当前指南,本文报告了接受 74 或 78 Gy EBRT 治疗的中危患者的长期预后。
Short Androgen Suppression and Radiation Dose Escalation in Prostate Cancer: 12-Year Results of EORTC Trial 22991 in Patients With Localized Intermediate-Risk Disease
在819位随机接受EBRT或EBRT联合AS(EBRT第一天)治疗的患者中,481位为中风险(国际抗癌联盟 TNM 1997 cT1b-c 或 T2a、前列腺特异性抗原[PSA]≥10 ng/mL,或Gleason≤7 和PSA ≤20 ng/mL,N0M0),其中342位(71.1%)的EBRT为74 Gy,139位(28.9%)的为78 Gy。主要终点是EFS、DFS、无远处转移生存期(DMFS)和总生存期(OS)。
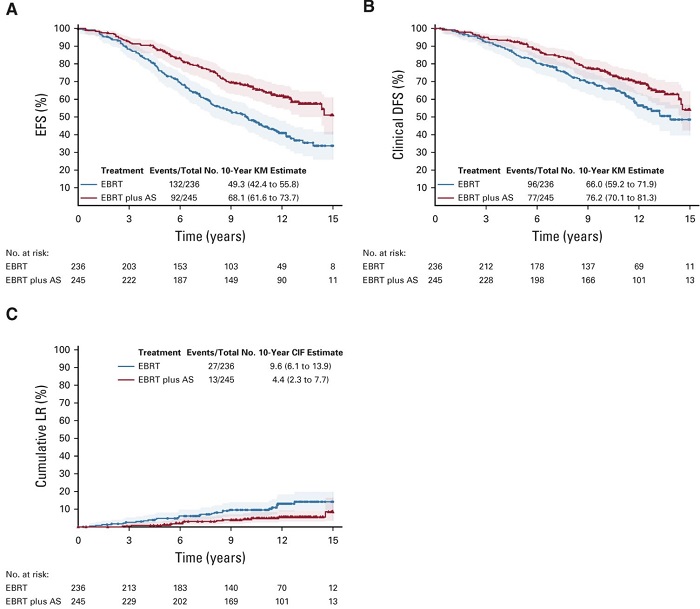
两组患者的EFS、DFS和累积LR
中位随访了12.2年后,EBRT+AS组245位患者中有92位获得了EFS事件,而EBRT组236位患者中有132位获得了EFS事件;大部分患者发生了PSA复发(48.7%)或死亡(45.1%)。与EBRT组相比,EBRT+AS组的EFS和DFS均明显提高(风险比[HR] 0.53;95%CI 0.41-0.70;p<0.001和0.67; 0.49-0.90; p=0.008)。随访10年时,EBRT+AS组和EBRT组的DMFS分别是79.3%和72.7%(HR 0.74; 95%CI 0.53-1.02; p0.065)。
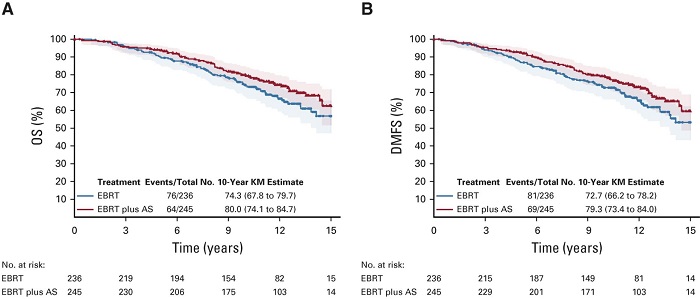
两组患者的OS和DMFS
随访过程中,共记录了140例死亡:EBRT+AS组 64例、EBRT组 76例。EBRT+AS组和EBRT组的10年OS分别是80.0%和74.3%,但无显著差异(HR 0.74; p=0.082)。
综上,6 个月的伴随和辅助 AS 治疗显著改善了接受 74 或 78 Gy 放射治疗的中危前列腺癌患者的 EFS 和 DFS,但对 OS 和 DMFS 无统计学显著性的影响。
原始出处:
Bolla Michel,Neven Anouk,Maingon Philippe et al. Short Androgen Suppression and Radiation Dose Escalation in Prostate Cancer: 12-Year Results of EORTC Trial 22991 in Patients With Localized Intermediate-Risk Disease.[J] .J Clin Oncol, 2021, undefined: JCO2100855. https://doi.org/10.1200/JCO.21.00855
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#长期预后#
28
#Oncol#
16
谢谢梅斯分享这么多精彩信息
50
前列腺癌相关研究,学习了,谢谢梅斯
41
好
47
关注医学
61