JCO:阿替利珠单抗(Atezolizumab)+贝伐珠单抗+化疗在初始诊断III或IV期卵巢癌中的疗效和安全性:安慰剂对照随机III期研究(IMagyn050/GOG 3015/ENGOT-OV39)
2021-06-09 yd2015 MedSci原创
现有证据不支持阿替利珠单抗(Atezolizumab)加入初始诊断FIGO III或IV期卵巢癌的标准治疗中。
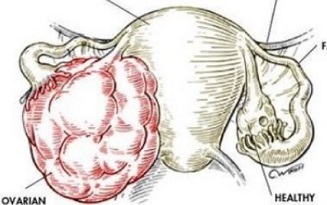
卵巢癌(OC)是女性常见的恶性肿瘤。标准治疗一般为手术联合铂类-紫杉类化疗。而在此基础上联合贝伐珠单抗可改善无进展生存期(PFS)和总生存期(OS)。阿替利珠单抗(Atezolizumab)是一种PDL1抑制剂,其联合治疗可以改善非小细胞肺癌和肝细胞癌患者的预后。但是阿替利珠单抗联合标准治疗在卵巢癌中的作用不清楚。近期,发表在Journal of Clinical Oncology杂志上的III期临床研究(IMagyn050/GOG 3015/ENGOT-OV39) (ClinicalTrials.govidentifier: NCT03038100)给出了答案。
该研究是多中心,安慰剂对照、双盲、随机对照III期临床研究。双研究终点为PFS和OS,次要终点为客观缓解率(ORR),缓解持续时间(DoR)和不良事件(AE)。纳入FIGO III或IV期OC患者,拟进行手术但伴有残留或新辅助化疗后手术。共纳入2017年3月8日至2019年3月26日期间1301例患者,随机分配为阿替利珠单抗治疗组651例患者,安慰剂对照组为650例患者。784例患者(60%)为PD-L1阳性。
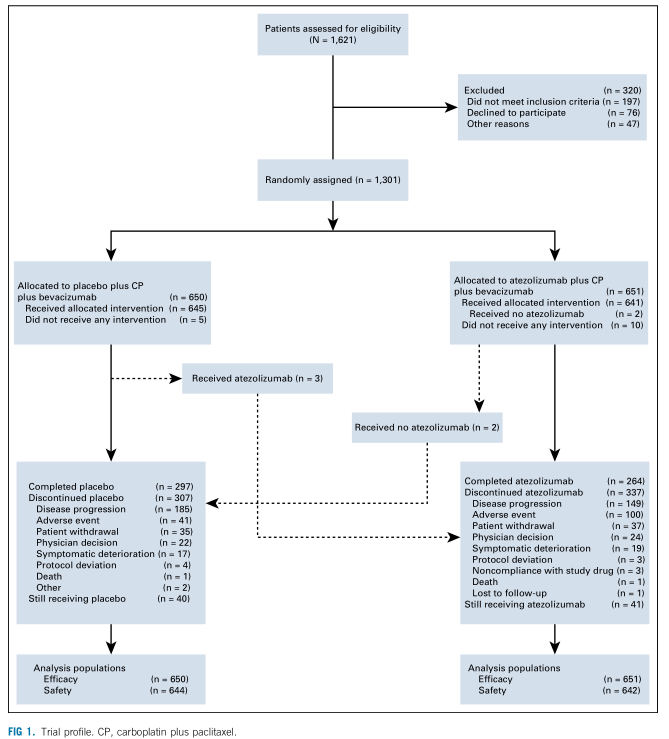
研究概况
意向性人群(ITT)分析,阿替利珠单抗组和安慰剂组的中位PFS分别为19.5个月(95% CI, 18.1 to 20.8) 和18.4个月(95% CI, 17.2 to 19.8)(HR=0.92,95% CI, 0.79 to1.07, P=0.28)。PD-L1阳性患者分析,阿替利珠单抗组和安慰剂组的中位PFS分别为20.8个月(95% CI, 19.1 to 24.2) 和18.5个月(95% CI, 16.6 to 21.4)(HR=0.8,95% CI, 0.65 to 0.99; P=0.038)。
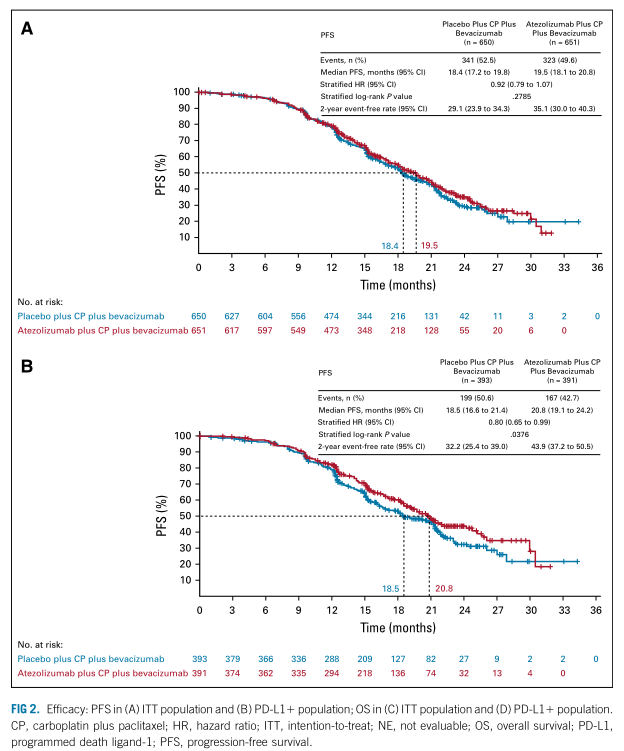
ITT人群和PD-L1阳性人群PFS
PFS分析时,中位OS尚未成熟。意向性人群(ITT)分析,阿替利珠单抗组和安慰剂组的2年OS率分别为81% (95% CI, 77 to 84) 和79% (95% CI, 75 to 83)。PD-L1阳性患者分析,阿替利珠单抗组和安慰剂组的2年OS率分别为82% (95% CI, 77 to 87) 和83% (95% CI, 78 to 87)。
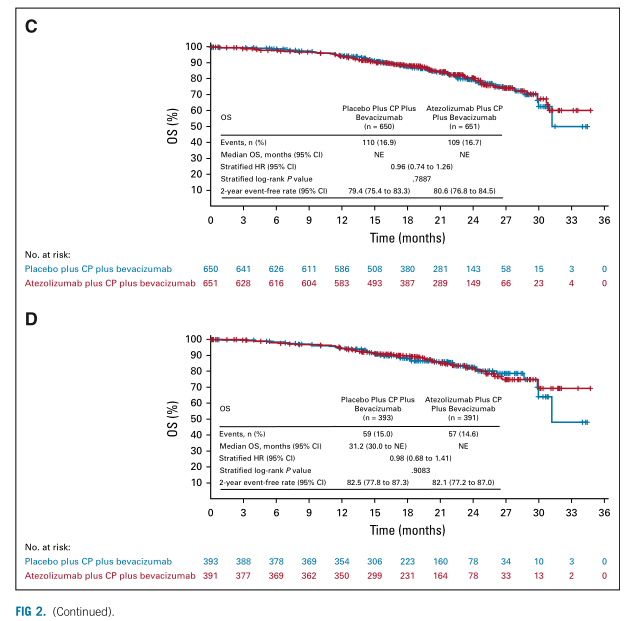
ITT人群和PD-L1阳性人群OS
意向性人群(ITT)中,阿替利珠单抗组中251例可评估患者中233例患者出现缓解(93%; 95% CI, 89 to 96),而安慰剂组中239例可评估患者中212例患者出现缓解(89%; 95% CI, 84 to 92)。PD-L1阳性患者中,阿替利珠单抗组中169例可评估患者中156例患者出现缓解(92%; 95% CI, 87 to 96),而安慰剂组中158例可评估患者中142例患者出现缓解(90%;95% CI, 84 to 94)。
免疫细胞(ICs)的PD-L1表达大于等于5%患者中,阿替利珠单抗组和安慰剂组的中位PFS分别为未达到和20.2个月 (95% CI,17.1 to 21.9)(HR=0.64,95% CI, 0.43 to 0.96)。肿瘤细胞(TCs)的PD-L1表达大于等于1%患者中,阿替利珠单抗组和安慰剂组的中位PFS分别为未达到和15个月(95% CI, 13.1 to 20.8)(HR=0.41,95% CI, 0.19 to 0.90)。
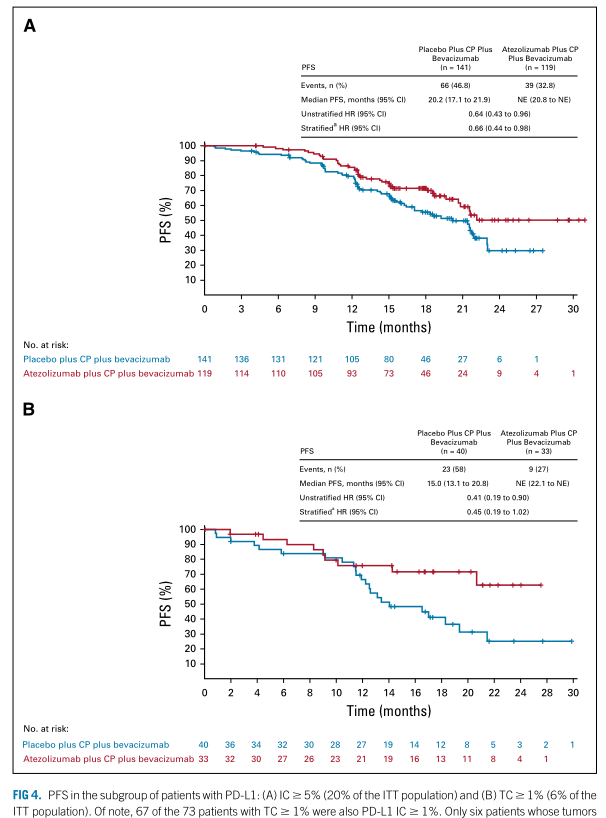
IC和TC 不同PDL1表达水平的PFS
3/4级AEs的发生在阿替利珠单抗组和安慰剂组分别为79%和73%。最常见的3/4级AEs为中性粒细胞减少(阿替利珠单抗组21%,安慰剂组21%),高血压(分别为18% v 20%)和贫血(12% v 12%)。
综上,现有证据不支持阿替利珠单抗(Atezolizumab)加入初始诊断FIGO III或IV期卵巢癌的标准治疗中。
原始出处:
Kathleen N Moore, Michael Bookman, Jalid Sehouli, et al. Atezolizumab, Bevacizumab, and Chemotherapy for Newly Diagnosed Stage III or IV Ovarian Cancer: Placebo-Controlled Randomized Phase III Trial (IMagyn050/GOG 3015/ENGOT-OV39). J Clin Oncol. 2021 Jun 10;39(17):1842-1855. doi: 10.1200/JCO.21.00306. Epub 2021 Apr 23.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#阿替利珠单抗#(Atezolizumab)+#贝伐珠单抗#+化疗在初始诊断III或IV期#卵巢癌#中的疗效和安全性,卵巢癌的难度还是相当大的,未来似乎要增加其它一些药物,如改善#肿瘤微环境#的药物,或抑制#细胞间液#生成的药物,象中医中#温阳化气#的,如#附子#,西药的#地高辛#这一类,可能有一定的辅助作用。
74
#JCO#
61
#疗效和安全性#
41
#III期研究#
48
#替利珠单抗#
44
#对照#
30
#III#
35
#mAb#
34
#贝伐珠#
34
#Eng#
36