NEJM:埃格列净不增加伴有动脉粥样硬化性心血管疾病的II型糖尿病患者的心血管风险
2020-09-24 MedSci原创 MedSci原创
对于伴有动脉粥样硬化性心血管疾病的II型糖尿病患者,埃格列净治疗后的心血管不良事件风险与安慰剂相当
近日研究人员评估了SGLT-2抑制剂埃格列净(Ertugliflozin)对II型糖尿病患者心血管风险的影响。
在这项多中心、双盲试验中,招募II型糖尿病伴有动脉粥样硬化性心血管疾病患者,随机每天一次接受5 mg 、15 mg的埃格列净或安慰剂。研究的主要终点为心血管不良事件,包括心血管疾病死亡、非致命性心肌梗死或非致命性中风死亡,次要结果是心血管疾病死亡或因心力衰竭住院。
8246名患者参与研究,平均随访3.5年,其中8238名参与者接受过至少一次埃格列净或安慰剂治疗,埃格列净组5493名患者中的653名(11.9%),安慰剂组2745名患者中的327名(11.9%)出现主要心血管不良事件(风险比0.97)。在埃格列净组5499例患者中,444例(8.1%)死于心血管疾病或因心力衰竭住院治疗,而安慰剂组2747例患者中有250例(9.1%,危险比为0.88)。埃格列净治疗后患者因心血管原因死亡的危险比为0.92,因肾脏原因死亡、肾脏替代治疗或血清肌酐水平加倍的危险比为0.81。54名(2.0%)接受5mg埃格列净治疗,57名(2.1%)接受15mg埃格列净治疗的患者(2.1%)进行了截肢,相比之下,45名接受安慰剂的患者(1.6%)进行了截肢。
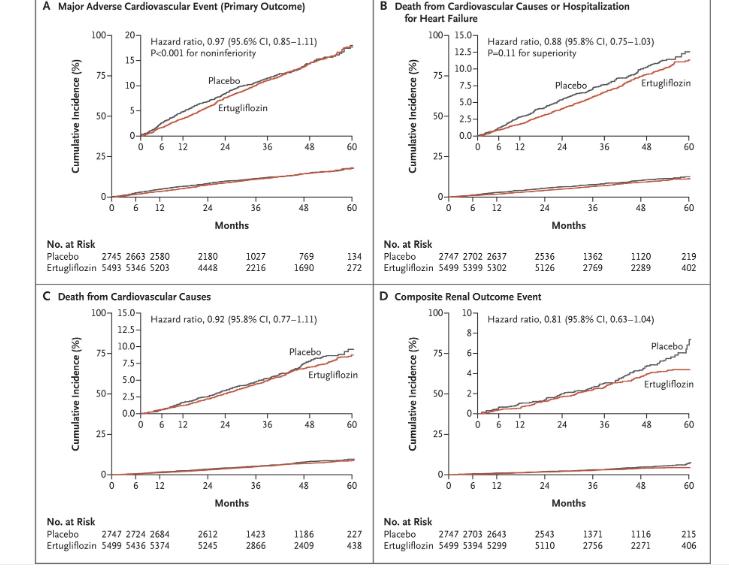
研究认为,对于伴有动脉粥样硬化性心血管疾病的II型糖尿病患者,埃格列净治疗后的心血管不良事件风险与安慰剂相当。
原始出处:
Christopher P. Cannon et al. Cardiovascular Outcomes with Ertugliflozin in Type 2 Diabetes. N Engl J Med, September 23, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#血管风险#
43
#粥样硬化#
47
#粥样硬化性#
53
#动脉粥样硬化性心血管疾病#
73
#II型糖尿病#
52
#糖尿病患者#
30
#硬化性#
33
#血管疾病#
34
不知道研究对象的地域,这篇文章对中国研究有没有帮助?
105
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
64