Ann Surg:微创食管切除术 vs 开胸食管切除术治疗的晚期食管癌患者的5年存活率
2021-01-25 MedSci原创 MedSci原创
晚期食管癌,该选择微创食管切除术还是开胸食管切除术?
食管癌是全球常见的癌症之一,5年总体存活率不足20%,是癌症相关死亡的第七大原因。无远处扩散的晚期食管癌多采用手术切除治疗,手术方式有微创食管切除术(MIE)和开胸食管切除术(OE)。本研究旨在比较两种手术方式后食管癌患者的5年存活率。
本研究是一项基于人群的队列研究,纳入2010-2016年间在瑞典或芬兰接受择期食管癌切除术的几乎所有患者,随访至2020年。
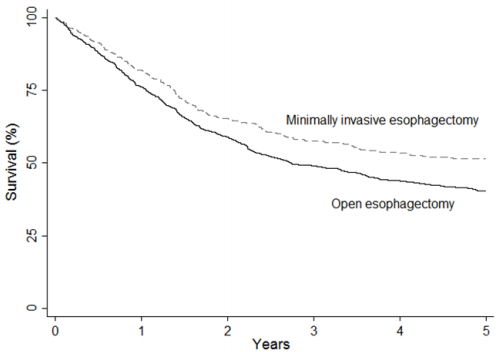
共1264例患者,其中470例(37.2%)接受了MIE,794例(62.8%)接受了OE。与OE相比,MIE与5年全因死亡率降低18%相关(校正风险比[HR] 0.82,95% CI 0.67-1.00;P=0.048)。混合MIE相比OE后的5年全因死亡率的校正HR为0.87(95% CI 0.68-1.11);而完全MIE相比OE后的全因死亡率的校正HR更低,仅为0.77(0.60-0.98)。
综上,这项两国研究表明,采用MIE治疗的食管癌患者的5年存活率明显高于采用OE治疗的患者,而且完全MIE比混合MIE对生存预后的好处更大。
原始出处:
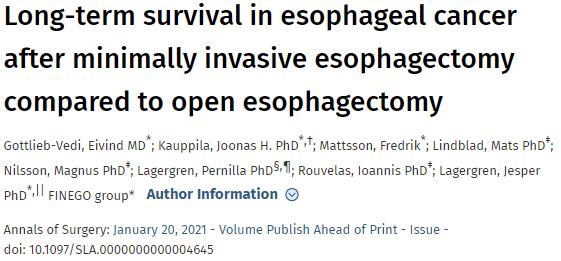
Gottlieb-Vedi Eivind,Kauppila Joonas H,Mattsson Fredrik et al. Long-term survival in esophageal cancer after minimally invasive esophagectomy compared to open esophagectomy. Ann Surg, 2021, https://doi.org/10.1097/SLA.0000000000004645.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#存活率#
50
#食管癌患者#
52
#切除术#
40
#食管切除术#
0
#微创#
37
#食管#
29
#晚期食管癌#
32
学习了
78
学习了
81