外伤性颈动脉海绵窦瘘误诊为眼眶蜂窝织炎1例
2019-04-16 冯子民 张四南 周小沅 中国临床神经外科杂志
男性,49岁,因左眼前突、红肿并疼痛3 d入住眼科。病人入院前3 d无明显诱因出现左眼红肿、疼痛伴睁眼困难,视物模糊、流泪、眼胀;无黑影飘动、视物变形、视野缺损,无眩光、眩晕及眼前闪光感,亦无夜昼盲、复视及结膜囊脓性分泌物等。
1. 病例资料
男性,49岁,因左眼前突、红肿并疼痛3 d入住眼科。病人入院前3 d无明显诱因出现左眼红肿、疼痛伴睁眼困难,视物模糊、流泪、眼胀;无黑影飘动、视物变形、视野缺损,无眩光、眩晕及眼前闪光感,亦无夜昼盲、复视及结膜囊脓性分泌物等。
眼科检查:左眼光感(无法矫正),色觉正常,光定位准确;眼球各方向运动受限,眼球前突,眼睑高度红肿、压痛,球结膜充血、水肿,部分球结膜脱出睑裂外,角膜雾浊,前房深浅正常,虹膜纹理清楚,无前后粘连;左侧瞳孔直径5 mm,对光反射消失。
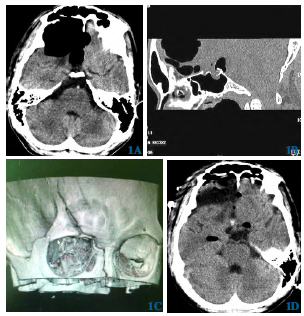
CT检查示左眼球突出,眼睑肿胀、增厚,眼外肌增粗,玻璃体、晶状体清晰,左眼球后脂肪组织内见少许絮状低密度影;MRI示左球后软组织肿胀,见片状长T1、长T2信号,正常眶壁骨质。CT、MRI考虑左眼球后炎性渗出,左眼眶蜂窝织炎。为排除颅内病变邀请神经外科会诊,体格检查:无波动性突眼,眼球触诊无震颤体征,眼部及全颅听诊未闻及杂音;左眼球固定,直接对光反射消失,间接光反射存在,否认颅内杂音。追问病史,4个月前曾驾驶摩托车摔伤左侧面部,伤后约1个月左眼有短暂(具体时间不详)胀痛不适,同期有无颅内杂音不确定;曾有多家眼科就诊史,相应治疗后眼部疼痛消失,未做进一步检查。
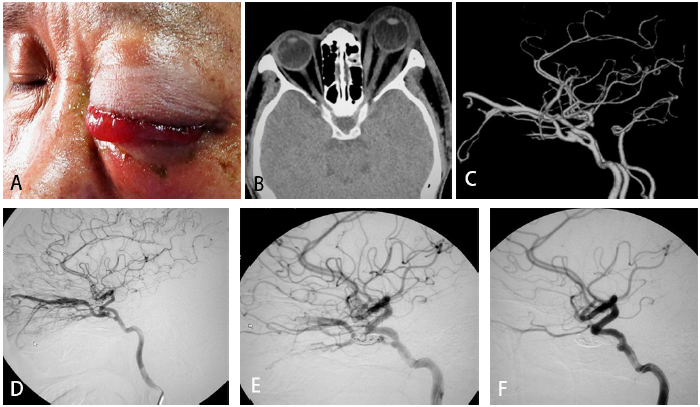
神经外科建议行CTA检查,结果示左眼眶见不规则片状软组织密度影包绕,其内见多支迂曲血管影,左眼上静脉增粗,呈动脉样强化,证实左侧颈动脉海绵窦瘘存在。行DSA检查:左颈内动脉远端供血良好,海绵窦段见一细小破裂口,眼静脉动脉化,周围毛细血管早期显影,同侧眼动脉显示不清,未见其他静脉及静脉窦引流。DSA确诊TCCF后,同期在气管插管全身麻醉下行海绵窦瘘栓塞治疗。考虑到瘘口较小,可脱球囊难以送入海绵窦腔,决定使用弹簧圈栓塞。
路径图引导下将Headway导管送入海绵窦腔,依次植入MicroPlex 18 7mm×30 cm弹簧圈3枚,造影见瘘口封堵不全,眼静脉仍有引流,但血流变缓,再注射Glubran2外科胶3 ml,再次造影见眼静脉引流消失,眼动脉显影良好,瘘口完全封堵。术后无并发症。术后1周结膜水肿消失,突眼症状明显减轻;睁闭眼自如,左侧瞳孔直径5 mm,无视力,直接光反射消失,间接光反射存在;右侧直接光反射存在,间接光反射消失。

图1 外伤性颈动脉海绵窦瘘栓塞治疗前后表现A. 栓塞前眼球前突结膜水肿;B. 栓塞前眼球CT 影像;C.栓塞前CTA,示海绵窦瘘小漏口;D. 栓塞前DSA,示眼静脉动脉化毛细血管扩张;E. 栓塞术中DSA,弹簧圈植入瘘口封堵不全;F. 栓塞后DSA,瘘口消失;G. 栓塞后1 周结膜水肿消褪突眼明显减轻
2. 讨论
2.1 海绵窦瘘分型
依据血管造影瘘口的解剖表现,Barrow 等将其分为A、B、C、D 四种类型,临床上Barrow A型最为常见,多与外伤有关。本文病例4个月前摔伤颅面部,病程中以眼部胀痛为主诉,直到入院前3 d方出现突眼、结膜水肿等症状,并且此时不伴有眼球搏动以及颅内杂音等TCCF典型症状,亦无颅内出血、缺血及蛛网膜下腔出血,始终以进行性视力下降而多家眼科就诊,均未考虑眼部以外疾病存在,直至误以“眼眶蜂窝织炎”住院治疗,后经CTA及DSA检查才最终确诊为Barrow A型海绵窦瘘。
2.2 治疗选择
TCCF治疗的主要目的在于保护和挽救视力,消除症状,防止脑出血或脑缺血,最佳治疗方法是既能闭塞瘘口,又能保留颈内动脉通畅,可脱性球囊栓塞技术已被国内外推荐为本病的首选治疗方法。对于非优势血流的海绵窦瘘、在无脑皮质静脉引流情况下,可采取保守治疗或间断压迫颈总动脉的方法,有10%~60%的病人病情可缓解甚至治愈,如果伴有皮层静脉引流,特别是已有出血者应视为颈总动脉压迫的禁忌症。
对于高流量TCCF应采取积极治疗措施,以避免灾难性后果。血管内可脱性球囊栓塞法为目前治疗TCCF首选,但对于小瘘口、流量较低TCCF来讲,目前可脱球囊难以漂入海绵窦腔内,从而有栓塞上的难度和局限性,单纯使用弹簧圈栓塞,费用较高。本文病例采用MicroPlex 187mm×30 cm弹簧圈辅助Glubran2外科胶栓塞达到满意治疗效果,既节约成本,亦降低费用。当然相同疾病可能有多种多样的并不完全一致的临床表现,选择何种治疗策略还要因病而异。
2.3 经验及教训
颅面部损伤(尤其是合并颅底骨折)后,出现搏动性突眼、颅内杂音、结膜水肿等典型症状,可确诊TCCF。需要注意的是,典型症状与动脉破口大小、位置以及静脉回流方向密切相关,当破口较小或者眼静脉为非优势引流时,TCCF主要症状可能并不同期发生,从而导致误诊。本文病例颅面部外伤后4个月内,始终未出现上述症状,反复以眼部疼痛不适、视力逐渐下降而多家眼科就诊,贻误最佳治疗时机,造成无可挽回后果。
经验与教训:①提高外伤性眼部疾病认识,警惕不典型TCCF。发生颅面部严重创伤后,与其相关学科都要高度重视,宜详细追问病史、注重诊断与鉴别诊断才能避免误诊误治。本例因延误治疗而失明,教训深刻。②高度重视病程中短暂、甚至是一过性症状体征并深入分析判断,对及时确定诊断有帮助。本文病例早期曾出现过夜间颅内杂音,但不久即消失,未引起足够重视,以至于多次就诊忽略这一重要症状,是误诊关键因素。③虽然CT(CTA)、MRI(MRA)、TCD可以辅助TCCF诊断,但金标准仍然是DSA。因此,若条件允许,被高度怀疑TCCF者,宜早期进行TCD、CTA或者DSA检查,送检时务必要重点描述主要症状、体征以及临床诊断意向,以供影像医师参考。本例影像误诊“左眼眶内蜂窝织炎”与缺少沟通不无关系。
总之,TCCF自然病程中少有自愈机会,一经诊断,应积极予以治疗,不管选用何种技术手段,要以消除异常动静脉交通、纠正海绵窦血流动力学异常、改善眼部症状以及防止脑出血或缺血、保证远端脑组织正常血供为原则,早期诊断、早期治疗是获得良好预后的关键与保证。对于小瘘口TCCF,电解脱弹簧圈辅以外科胶注射栓塞效果良好,且安全可靠,不但提高手术成功率,而且亦降低治疗成本。
原始出处:
冯子民,张四南,周小沅.外伤性颈动脉海绵窦瘘误诊为眼眶蜂窝织炎:1例报道及文献复习[J].中国临床神经外科杂志,2018(04):268-270.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#外伤性#
38
#颈动脉#
33
#眼眶#
41
学习
66