Lancet Oncol:中山大学肿瘤医院郭翔教授团队通过3期试验证实第三代铂类药物洛铂可有效治疗局部晚期鼻咽癌!
2021-04-21 Nebula MedSci原创
中山大学肿瘤医院郭翔教授团队通过3期临床试验证实第三代铂类药物洛铂可有效治疗局部晚期鼻咽癌!
《国家综合癌症网络指南》建议,使用以顺铂为基础的诱导化疗加同步放化疗治疗局部晚期的鼻咽癌。但是,顺铂与患者的依从性差有关,并具有明显的副作用。
第三代铂类药物,洛铂(Lobaplatin),在多种恶性肿瘤中显示出有希望的抗肿瘤活性,且毒性较低。
中山大学附属肿瘤医院鼻咽科主任郭翔教授及其同事率团队,在中国的5家医院开展了一项开放标签、非劣效性的随机对照3期临床试验,旨在评估以洛铂为基础的诱导化疗+同步放化疗 vs 以顺铂为基础的治疗方案用于局部晚期鼻咽癌的疗效。研究结果于近期发表在柳叶刀子刊”Lancet Oncology“上。
该试验招募了18-60岁的既往未治疗过的III-IVB期的鼻咽癌患者,且要求Karnofsky表现状态评分≥70分,血液和肝肾功能良好。受试患者被1:1随机分至两组,接受以洛铂或以顺铂为基础的诱导化疗,继以同步相同方案化疗+放疗。主要终点是5年无进展存活率。
2013年6月7日-2015年6月16日,评估了515位患者后,502位被招募入组:252位被分至洛铂组,250位被分至顺铂组。
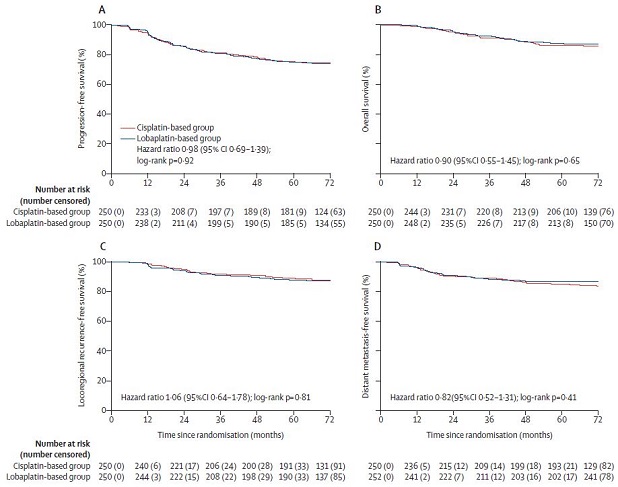
意向治疗人群预后
意向治疗人群中位随访了75.3个月后,洛铂组和顺铂组的5年无进展存活率分别为75%(95% CI 69.7-80.3)和75.5%(70.0-81.0;风险比[HR] 0.98,95% CI 0.69-1.39;p=0.92),差异为0.5%(95% CI -7.1~8.1;p=0.0070)。
在按协议治疗人群中,洛铂组和顺铂组的5年无进展存活率分别为74.8%(95% CI 69.3-80.3)和76.4%(70.9-81.9;HR 1.04, 95% CI 0.73-1.49;p=0.83),差异为1.6%(95% CI -6.1~9.3;p=0.016)。
在意向治疗人群中,洛铂组252位患者和顺铂组250位患者中各有63位(25%)获得了无进展生存事件;在按协议治疗人群中,洛铂组246位患者中有62位(25%)和顺铂组237位患者中有58位(25%)获得了无进展存活事件。
不良事件
最常见的3-4级不良事件有黏膜炎(洛铂组 vs 顺铂组:41% vs 40%)、白细胞减少症(16% vs 23%)和中性粒细胞减少症(10% vs 24%)。无治疗相关死亡。
综上所述,以洛铂为基础的诱导化疗联合同步放化疗用于局部晚期鼻咽癌患者的疗效不劣于以顺铂为基础的治疗方案,而且毒副作用更小。该试验结果提示,以洛铂为基础的诱导化疗联合同步放化疗或可成为这类患者的候选治疗方案。
原始出处:
Xing Lv, et al. Induction chemotherapy with lobaplatin and fluorouracil versus cisplatin and fluorouracil followed by chemoradiotherapy in patients with stage III–IVB nasopharyngeal carcinoma: an open-label, non-inferiority, randomised, controlled, phase 3 trial. The Lancet Oncology. April 12, 2021. https://doi.org/10.1016/S1470-2045(21)00075-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#铂#
37
#Oncol#
0
#Lancet#
35
#局部晚期#
40
#肿瘤医院#
51
#局部#
29
#3期试验#
51
#中山大学#
49
#铂类#
32
#有效治疗#
27