JACC:扩张型心肌病导致的复发性室速患者的临床预后
2022-09-12 MedSci原创 MedSci原创
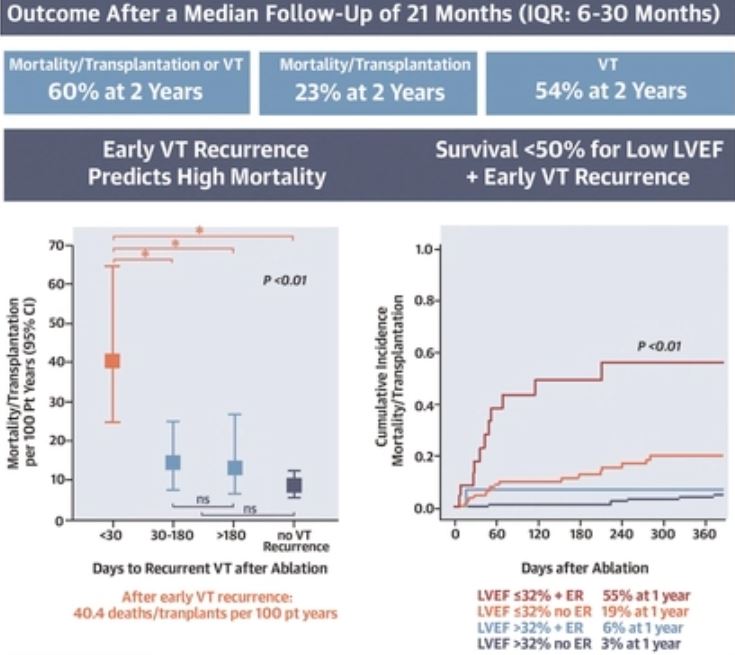
早期复发且LVEF≤32%的患者的一年死亡或心脏移植率高达55%
扩张型心肌病 (DCM) 导致的复发性室性心动过速 (VT) 比较难治疗,而且目前这类患者的长期预后数据比较缺乏。
该研究目的是确定这类复发性室性心动过速患者的死亡率或心脏移植(HTx)率,以及室性心动过速的复发率。
从9个医疗中心前瞻性的招募了进行室性心动过速射频导管消融 (RFCA) 的DCM患者,并进行随访。
共纳入了281位DCM患者(平均年龄:60±13岁,85%的男性,平均左心室射血分数[LVEF]:36%±12%),35%的患者有室速风暴,20%的患者有持续性室速,68%的患者用胺碘酮不能成功复律。
随访21个月后的临床预后
在21个月(IQR 6-30个月)的随访过程中,67位(24%)患者死亡或进行了心脏移植,138位(49%)患者室速复发(45位是在30天内,定义未早期复发);室速复发或死亡或心脏移植的4年发生率是70%。死亡或心脏移植的独立预测因素有室速早期复发(HR 2.92, p<0.01)、出院时使用胺碘酮(HR 3.23, p<0.01)、肾功能不全(HR 1.92,p=0.046)和LVEF(HR 1.36, p=0.052)。LVEF≤32%的患者有死亡或心脏移植的风险(曲线下面积:0.75)。
导管射频消融后,早期复发室速后的死亡或心脏移植的发生率是40.4例/100人·年,而晚期室速复发和无室速复发的患者的只有14.2例/100人·年和8.5例/100人·年(p<0.01)。早期复发且LVEF≤32%的患者的一年死亡或心脏移植率高达55%。前置式心律转复除颤器电击、基础室间隔前室速起源和手术失败可预测VT复发,但不能预测LVEF。
综上,需要导管射频消融治疗室速的扩张型心肌病患者是一个高危的人群。导管射频消融后,大约一半的患者会复发室速。早期复发且LVEF≤32%的患者具有高死亡和心脏移植风险,应考虑及时进行机械支持或心脏移植筛查。
原始出处:
Katja Zeppenfeld, et al. Clinical Outcomes in Patients With Dilated Cardiomyopathy and Ventricular Tachycardia. J Am Coll Cardiol. 2022 Sep, 80 (11) 1045–1056
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#扩张#
43
#复发性#
68
#JACC#
50
#ACC#
56
#室速#
57
#临床预后#
35
#肌病#
42