Hypertension:根据年龄的血压对糖尿病患者终末期肾脏病的影响
2022-05-31 MedSci原创 MedSci原创
较高的收缩压和舒张压会增加糖尿病患者发生终末期肾病的风险,特别是年轻患者将面临更大的风险。
糖尿病是终末期肾脏疾病(ESRD)的一个重要危险因素。高血压在肾衰竭的发生发展中也起着至关重要的作用。随着肾功能下降,血压升高,进而加重高血压。此外,随着慢性肾脏疾病(CKD)的恶化,血压变得更难控制,血压升高和肾功能恶化之间形成恶性循环。因此,对高危高血压患者进行早期诊断和及时治疗至关重要。然而,并没有针对年龄或收缩压和舒张压的具体高血压治疗指南。

近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员旨在评估年龄相关性血压对糖尿病患者终末期肾脏疾病(ESRD)发生发展的影响。
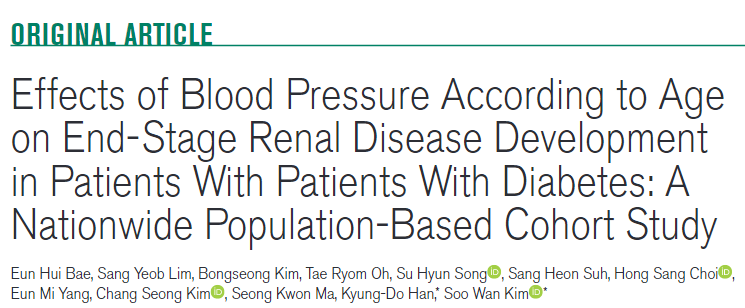
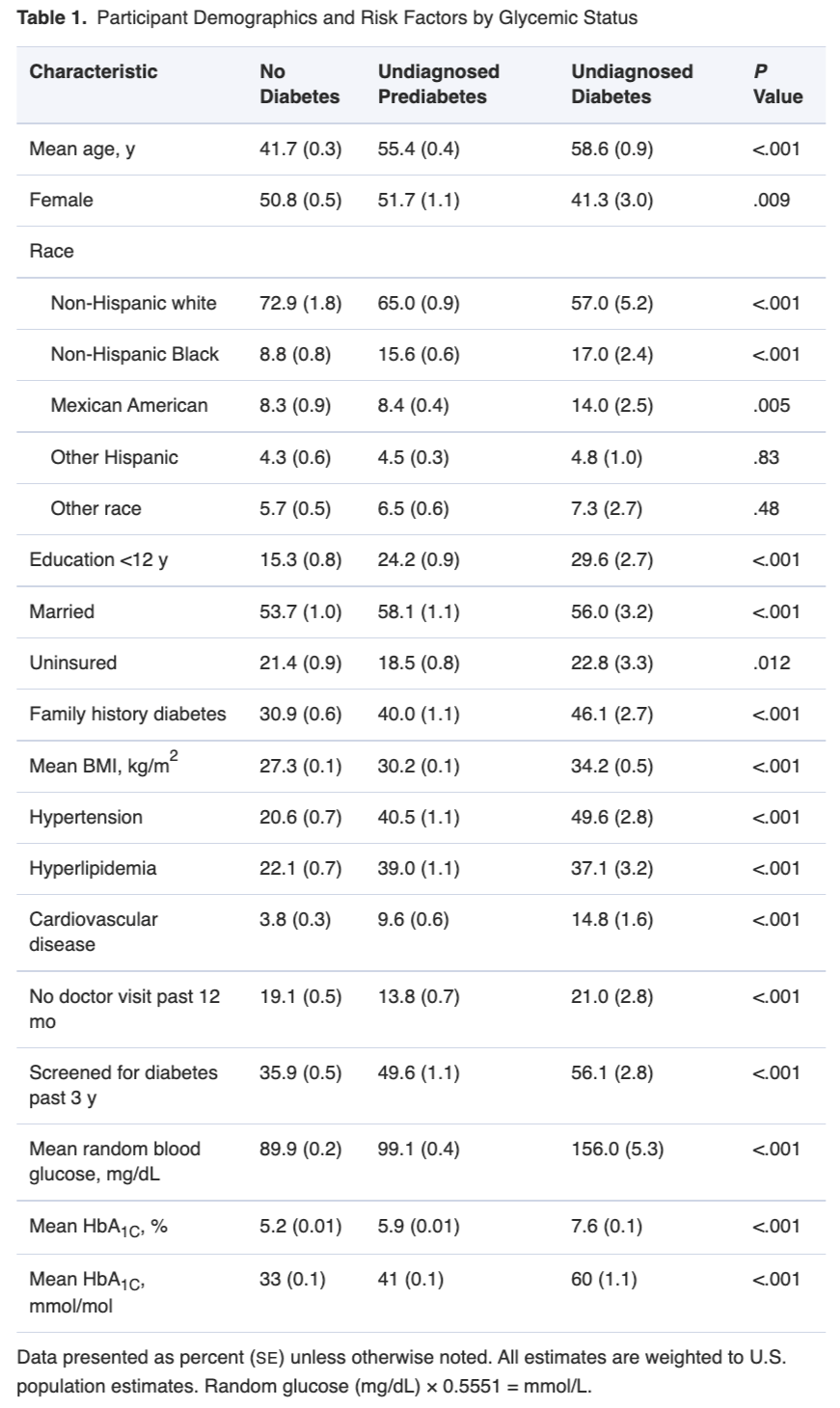
从2009年到2012年期间,研究人员从韩国国家健康筛查项目中选择了2563870名年龄20岁以上的糖尿病患者,并随访到2019年底。研究人员将参与者按年龄和血压进行分组,并计算了ESRD的风险比。
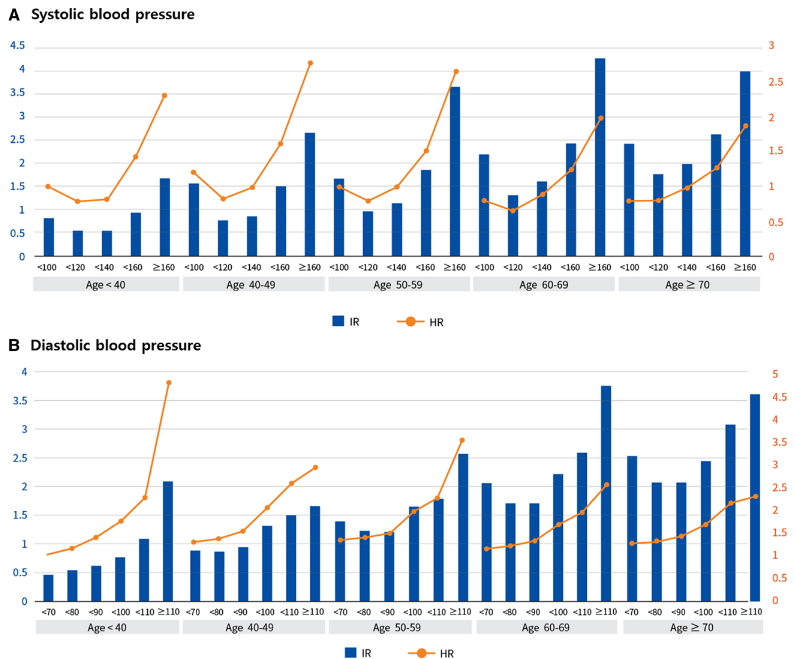
在7.15年的中位随访期间,ESRD的发生率随着收缩压和舒张压的增加而增加。年龄小于40岁且舒张压≥100mmHg的患者ESRD的风险比最高。收缩压和舒张压对ESRD发展的影响随年龄的增长而有所减弱(年龄和收缩压的交互作用P<0.0001,年龄和舒张压的交互作用P<0.0022)。性别、降压药物、慢性肾脏病史亚组分析显示,年龄小于40岁、未服用降压药物、有慢性肾脏病的男性发生ESRD的风险比高于女性、年龄大于40岁、服用降压药物和非慢性肾病组。
由此可见,较高的收缩压和舒张压会增加糖尿病患者发生终末期肾病的风险,特别是年轻患者将面临更大的风险。因此,在年轻患者中加强血压管理是必要的,以预防ESRD。
原始出处:
Eun Hui Bae.et al.Effects of Blood Pressure According to Age on End-Stage Renal Disease Development in Patients With Patients With Diabetes: A Nationwide Population-Based Cohort Study.Hypertension.2022.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.121.18881
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
31
#TENS#
42
#终末期#
41
看来血压一定要控制好
44
学习
44
学习
46
#糖尿病患者#
26
#Hypertension#
41