Gastroenterology:炎性肠病中血栓栓塞性疾病的发生率以及遗传风险对其的影响
2021-02-25 MedSci原创 MedSci原创
炎症性肠病(IBDs)主要包括克罗恩病(CD)和溃疡性结肠炎(UC),它是一组胃肠道相关的慢性复发性炎症。
炎症性肠病(IBDs)主要包括克罗恩病(CD)和溃疡性结肠炎(UC),它是一组胃肠道相关的慢性复发性炎症。IBD的发病率正在逐年增加,美国的患病率> 1.3%,全球患病率超过0.3%。据报道,IBD患者的血栓栓塞性疾病(TED)发生风险相比于普通人增加3到4倍,TED也是IBD相关死亡的主要原因。这种增加的风险似乎是IBD所独有的,因为其他慢性炎症性疾病(例如类风湿关节炎和腹腔疾病)不会带来这种风险。

许多因素可以影响TED风险的增加,包括疾病活动,住院,年龄,怀孕,药物,手术和遗传因素。先前有关IBD患者TED遗传风险的报道主要集中在单基因变异体上,例如因子V Leiden缺乏症。随着对TED的遗传病因学的日益了解以及基因分型/测序的成本不断降低,通过遗传学评估TED风险正在成为一种可行的临床工具。因此,本项研究的目的是利用全外显子组测序和全基因组基因分型来确定遗传上有TED风险的IBD患者比例,并研究TED遗传在IBD中的风险差异。
研究方案如下:首先TED的多基因风险评分由全基因组基因分型计算得出,纳入的患者主要是从全外显子组测序中提取出血友病致病性变异体的患者。共有792名IBD患者拥有全外显子组测序和基因分型数据。如果TED多基因风险评分高或携带至少1种血友病致病性变异,便将其定义为TED遗传风险高的患者。
792名IBD患者中有122名(15.4%)为TED的遗传高风险患者。715名患者拥有完整的电子病例数据,其中有63名(8.8%)发生了TED事件。遗传基因中高风险TED患者与TED事件的真实发生存在显着相关性(OR:2.5;P = .0036)。此外,本项研究还证实了单基因和多基因风险对TED具有累加效应(P= .0048)。相较于TED遗传风险低的患者,TED遗传风险高的患者易发生多处血栓(78%vs 42%,HR,3.96;P= .048)。
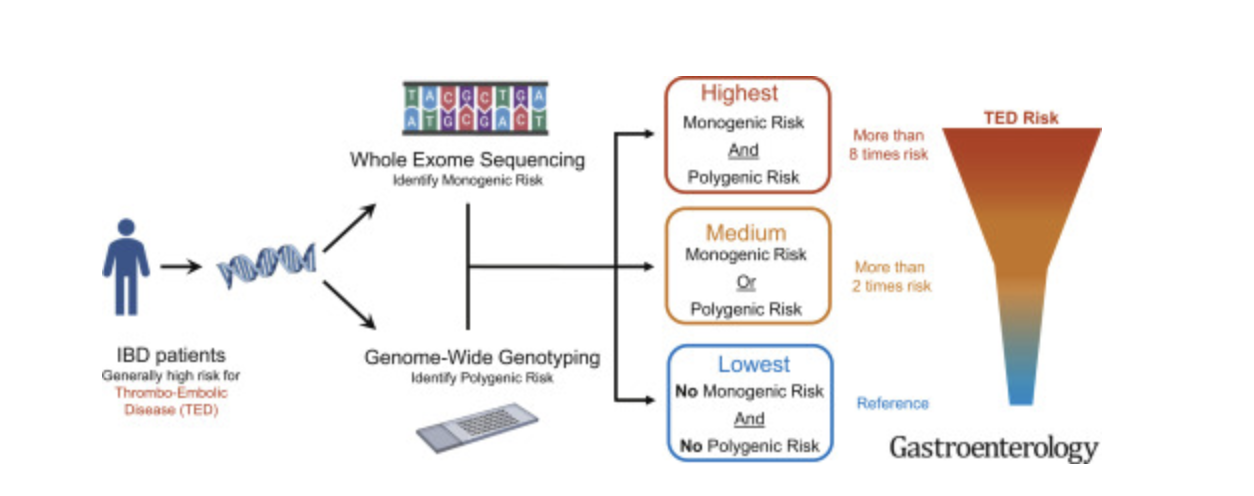
本项研究证实:遗传风险(多基因和单基因)与TED发生几率显着相关。遗传学特征识别出高风险患者发生TED风险比低风险患者高2.5倍或更高。
原始出处 :
Takeo Naito. Et al. Prevalence and Effect of Genetic Risk of Thromboembolic Disease in Inflammatory Bowel Disease. Gastroenterology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#AST#
34
#发生率#
24
#Gastroenterol#
24
#GAS#
30
#遗传风险#
38
#Gastroenterology#
22