Multiple Sclerosis Journal:脑桥周围病变的定位是鉴别MS与小血管病的良好指标
2021-06-30 MedSci原创 MedSci原创
脑桥周围病变的定位是鉴别MS与小血管病的良好指标。
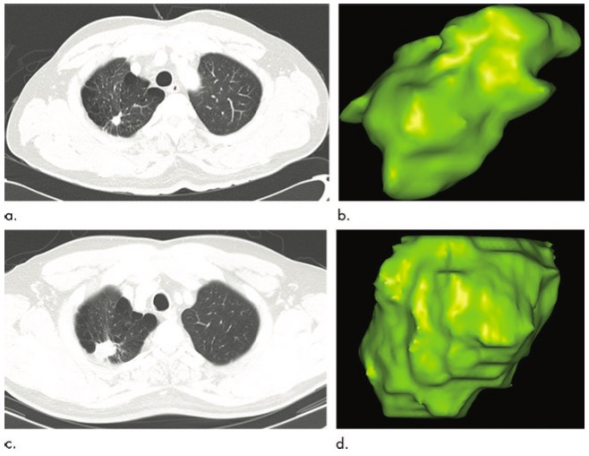
多发性硬化症(MS)中描述了桥脑周围的病变,理论上,由于丰富的血管化,该区域不易发生血管危险因子(VRF)相关的小血管病(SVD)。相反,中央桥由穿通端小动脉供应,易发生缺血缺氧和脱髓鞘,这是VRF-SVD患者T2磁共振成像(MRI)高信号的基础。然而,这些假设是基于有限的观察和这些标志物在鉴别MS和SVD相关病变中的作用还没有得到验证。 Ruth Geraldes等探讨了VRFs和MS是否与位于不同位置的脑桥病变相关,定义为中心或周围,并确定这些位置的脑桥病变对MS和VRF-SVD的特异性。研究结果发表在Multiple Sclerosis Journal杂志。 将多发性硬化(MS)与血管危险因素(VRF)-小血管疾病(SVD)区分开来是一个具有挑战性的问题。 为了确定脑桥病变的位置是否是鉴别MS和VRF-SVD的有用指标,该研究对93例无VRF的MS患者、108例VRF的MS患者和43例VRF的非MS患者的脑桥病变进行了脑磁共振(MRI)分类。 (a) 如果脑桥病变位于脑桥中点(从基底沟到后正中沟的一条线的中点,如轴向切面所见)半径为1.0 cm,则为中央型;如果超出该半径,则为外
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血管病#
48
#小血管病#
40
#Sclerosis#
37
#良好指标#
33
#脑桥#
53
#ROS#
36