JNNP:ChAdOx1 nCov-19疫苗接种后脑静脉窦血栓形成的临床和生物学特征
2021-10-11 MedSci原创 MedSci原创
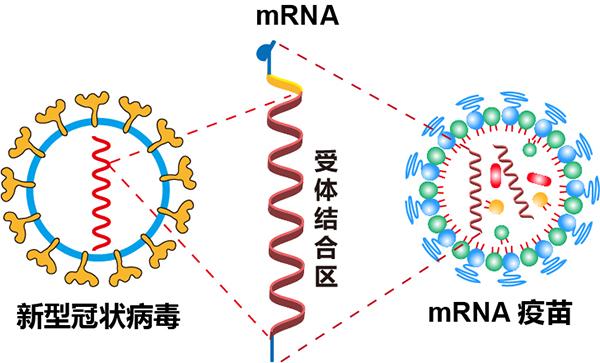
新冠病毒-19疫苗的开发速度前所未有,自2021年1月以来,阿斯利康/牛津大学ChAdOx1 nCoV-19疫苗已在全球4亿多人中接种。 欧洲药物和保健品管理局(MHRA)于2021年4月报
新冠病毒-19疫苗的开发速度前所未有,自2021年1月以来,阿斯利康/牛津大学ChAdOx1 nCoV-19疫苗已在全球4亿多人中接种。 欧洲药物和保健品管理局(MHRA)于2021年4月报告了ChAdOx1 nCoV-19接种后出现罕见部位血栓形成合并血小板减少综合征(称为疫苗诱导免疫性血栓性血小板减少症(VITT))。VITT的频率因年龄组而异。截至2021年7月21日,MHRA共报告了411例VITT病例,病死率为17.76%(73/411)。

报告了来自英国伦敦一个三级转诊中心的四例VITT患者的经验,他们患有脑静脉窦血栓形成(CVST)并伴有或不伴有其他地方的血栓形成。所有患者在发表前均获得知情书面同意。所有患者均符合VITT的拟定诊断标准。本文发表在《神经病学,神经外科学和精神病学杂志》上()。
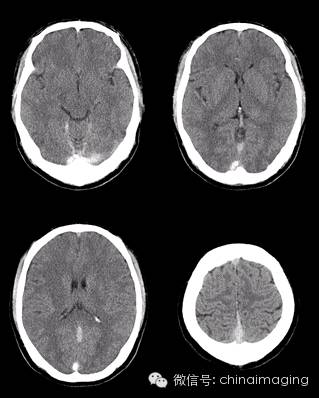
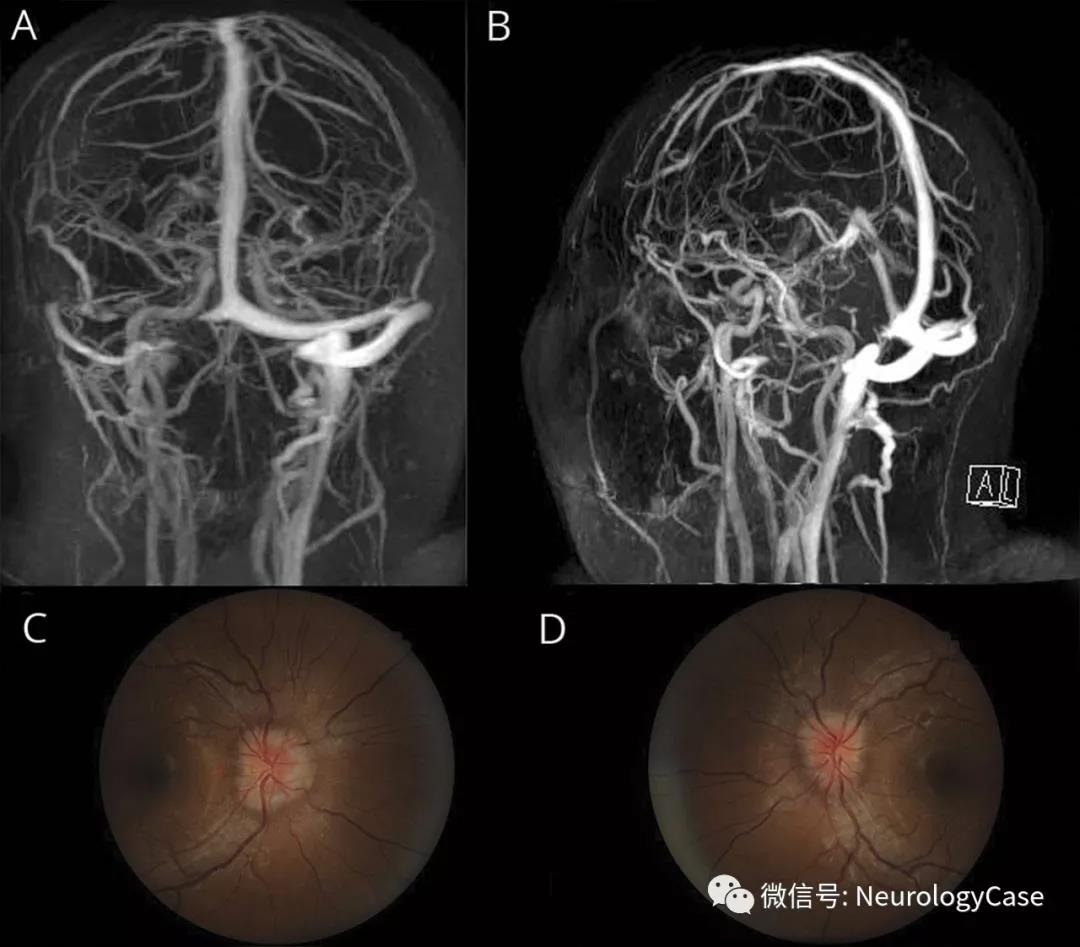
所有四名患者均为41-46岁的女性,在ChAdOx1 nCov-19疫苗接种后7-28天诊断为VITT。每个人都表现为头痛和不同程度的神经功能缺损。患者1的神经成像显示广泛的血栓形成,累及硬脑膜静脉窦和皮质浅静脉,以及双侧壁沟相关的蛛网膜下腔出血,但在腹部成像中未检测到血栓形成。患者2最初表现为上矢状窦血栓形成,伴有右侧神经功能缺损、肝内门静脉分支血栓和与肺栓塞(CT肺血管造影(CTPA))一致的非闭塞性节段性肺动脉充盈缺损。2周后进行的CT静脉造影(CTV)显示,随着血栓大小的减小,情况有所改善。在患者3中,CTV显示广泛的硬脑膜静脉窦血栓影响上矢状窦、左横窦和乙状窦,CTPA显示一个巨大的鞍状栓子,广泛的血栓延伸到两侧的所有叶支,具有右心劳损的特征,MRI进一步显示了血栓形成的皮质静脉和蛛网膜下腔出血的多个部位。对于患者4,CTV显示广泛的CVST,左后颞叶继发梗死/水肿。腹部CT扫描显示门静脉和肝静脉血栓。
四例脑静脉窦血栓形成疫苗诱导的免疫性血栓性血小板减少症患者的头颅影响
四分之三和四分之二的患者分别出现血小板减少和低纤维蛋白原血症,并且所有四名患者的D-二聚体均显著升高。确认选择合适的抗血小板因子4(PF4)抗体试验5的重要性,因为所有患者在AcuStar HIT IgG(PF4-H)化学发光试验中均呈阴性,但在两种抗PF4 ELISA(Immucor,Hyphen BioMed)中呈强阳性。额外的自身抗体检测显示,患者2和患者4的抗核抗体水平较低,而在9种不同的aPL检测中均未检测到抗磷脂(aPL)抗体(IgG、IgM、IgA抗心磷脂和抗-ß2GPI;IgG抗-ß2GPI结构域I;IgG、IgM抗磷酰丝氨酸/凝血酶原)。因此,结果强化了抗PF4是VITT关键致病性抗体的结论。
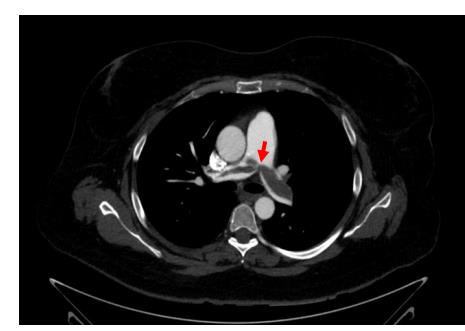
主肺动脉水平的CT图像
采用统一的治疗方法,紧急血浆置换(PLEX)与静脉注射免疫球蛋白(IVIg)、高剂量类固醇联合使用(静脉注射1 g甲基强的松龙,然后静脉注射或口服20 mg地塞米松,持续4天,并在接下来的几天内逐渐减少剂量)和含利妥昔单抗的非肝素抗凝剂(最初为阿加曲班)(375 mg/m2)。所有四名患者均存活,症状完全消失,实验室标记物支持该治疗方法,目前估计该综合征的死亡率为70%,尤其是有出血证据的患者。脑梗死转化为出血是公认的并发症严重的血小板减少和低纤维蛋白原血症以及抗凝治疗的需要可能会加剧CVST的恶化。
本文介绍的四例患者的治疗代表了一种积极的VITT治疗方法,这在患者的良好预后中起到了核心作用。所有四名患者的血管性血友病因子抗原和活性以及纤溶酶原激活物抑制剂-1水平均显著升高。循环因子VIII、血栓调节蛋白、E-选择素、细胞间粘附分子-1、血管细胞粘附分子-1和P-选择素也有不同程度的升高。综上所述,这些发现提示正在进行纤溶,并提示血小板和内皮细胞的炎症反应。相比之下,凝血酶原时间、活化部分凝血活酶时间、抗凝血酶、蛋白S和蛋白C的测量结果并不显著,表明患者没有发生弥散性血管内凝血。考虑到非常高的D-二聚体和减少的纤维蛋白原,这有点令人惊讶,因此必须反映局部纤维蛋白的形成和分解。
这是第一项结合VITT成像研究免疫、凝血/止血、血小板和内皮功能障碍的研究。本文报告的结果表明,针对发病机制的快速攻击性治疗可能是有益的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#静脉#
37
#生物学特征#
49
#静脉窦血栓#
50
#ChAdOx1#
40
#疫苗接种#
37
#生物学#
36
#静脉窦#
32