DCR: 灌洗细胞学检查在预测结直肠癌的发病率和预后价值
2022-06-28 xuyihan MedSci原创
腹腔灌洗是通过长时间的有效的冲洗以及持续低负压的吸引,将腹腔内的积血、积液、积脓液以及坏死组织等物质引出体外,减少毒素的吸收,并防止感染。
在结直肠癌(CRC)的分期中,国际抗癌联盟(UICC)发布的TNM分类标准已得到广泛的认可,这个分期主要由原发肿瘤、淋巴结转移、远处转移三个因素组成。腹膜转移也被认为是远处转移因素之一。在胃癌患者中,用于检测腹腔内游离癌细胞的灌洗细胞学 (LCY) 已被广泛应用于预测腹膜内微转移,但是LCY在CRC中的临床意义尚未确定。本研究旨在探讨灌洗细胞学阳性对结直肠癌患者预后的影响。

这是一项单机构的回顾性观察研究,研究人员回顾性分析2007年至2013年的3135例结直肠癌病例。术中腹膜冲洗细胞学检查在手术开始后进行,然后将冲洗液以每分钟 2500 转的速度离心5分钟,将细胞团块涂抹在显微镜载玻片上,并进行巴氏染色。主要观察结果是5年总生存率。次要观察结果是5年复发率。
研究结果显示在19例(2.0%)和86例(16.9%)III 期和 IV 期结直肠癌病例中检测到灌洗细胞学阳性;然而,在 I 期和 II 期结直肠癌中没有发现阳性病例。在多变量分析中,灌洗细胞学阳性是 III 期和 IV 期结直肠癌的独立预后因素(III 期 5 年死亡率 HR 3.59 [1.69-7.64],IV 期 2.23 [1.15-4.31])。III期和IV期灌洗细胞学阳性组的5年生存率预后明显较差。在复发方面,III期灌洗细胞学阳性组与IV期灌洗细胞学阳性/阴性组的结果相似(73.7%、70.0%和75.0%)。
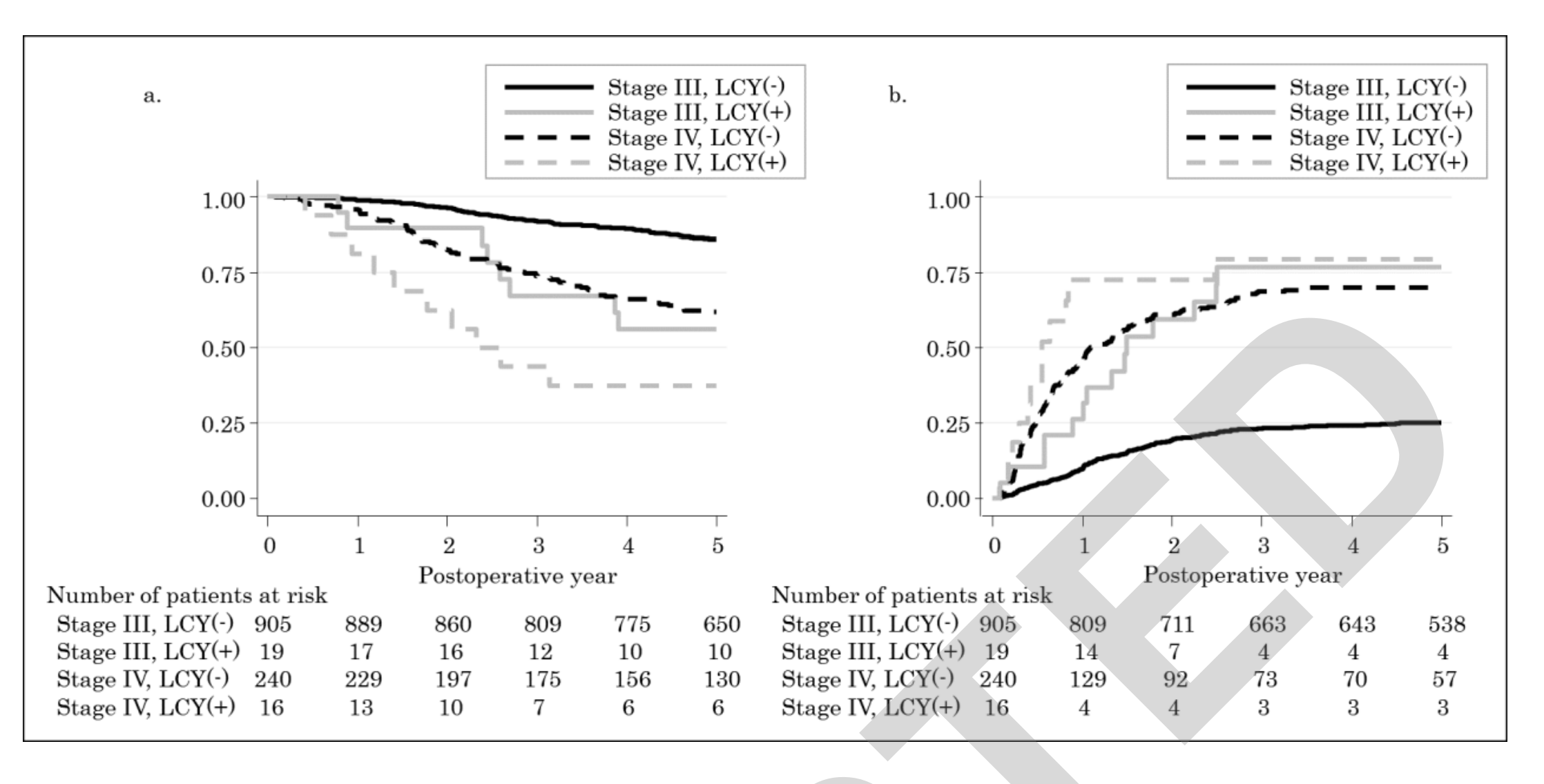
由于淋巴结转移和淋巴血管侵犯可以预测CRC的复发,而本项研究证实灌洗细胞学阳性更能够敏感判断IV期结直肠癌的预后因素。
原始出处:
Matsui, Shimpei. Et al. Incidence and Prognostic Value of Lavage Cytology in Colorectal Cancer. Diseases of the Colon & Rectum.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞学检查#
33
#细胞学#
38
#发病率#
0
不错学习了。
41
#预后价值#
32
#结直肠#
28