IBD:单核细胞增多症是炎症性肠病严重程度的生物标志物
2022-01-13 MedSci原创 MedSci原创
溃疡性结肠炎是一种病因尚不十分清楚的结肠和直肠慢性非特异性炎症性疾病,病变局限于大肠黏膜及黏膜下层。病变多位于乙状结肠和直肠,也可延伸至降结肠,甚至整个结肠。
溃疡性结肠炎(UC)和克罗恩病(CD)是一组异质性的免疫介导的慢性胃肠道炎症性肠病(IBD)。在UC和CD中,临床表型是不同的,有不同的疾病轨迹、结果和对治疗的反应。鉴于IBD表型的多样性和疾病严重程度的影响,如何识别高风险患者,使其从积极的治疗中获益最多,仍是一个挑战。识别与疾病严重程度相关的生物标志物对于指导临床医生的临床实践和为每个病人提供个性化治疗至关重要。
单核细胞是循环白细胞的一个亚群,在先天性疾病中发挥重要作用,它能够通过血液被输送到外周组织,在细胞因子或微生物分子的刺激下,分化成巨噬细胞和树突状细胞。有证据表明,与健康对照组患者相比,IBD患者的外周单核细胞的表型发生了改变。有人认为单核细胞增多症与UC患者的疾病活动有关,但在CD中还没有进行过研究。本研究的目的是确定单核细胞增多症与炎症性肠病疾病严重程度之间的联系。
为此,研究人员收集了2010年1月至2015年12月间在医疗结构接受治疗的炎症性肠病患者的临床资料。单核细胞增多症被定义为单核细胞绝对计数超过正常值的上限,然后在所有患者中按疾病类型比较了单核细胞增多症的 IBD 患者与无单核细胞增多症的患者之间的相关性。
本项研究共纳入1290名IBD患者(64.1% 患有克罗恩病;35.9% 患有溃疡性结肠炎)(平均年龄46.4岁;52.6%为女性)。研究人员在399 名 (30.9%) 的 IBD 患者(29.3% 患有克罗恩病;33.9% 患有溃疡性结肠炎)发现了单核细胞增多症的症状。单核细胞增多症与异常 C 反应蛋白水平和红细胞沉降率、贫血、较差的生活质量、活动性疾病和生物制剂暴露增加显着相关(P< 0.001)。与没有单核细胞增多症的患者相比,单核细胞增多症患者的年度财务医疗保健费用增加了3倍(中位数:127,013 美元 VS 32,925 美元,P< 0.001)和住院可能性增加(AOR,4.5;P< 0.001)、以及IBD 相关手术 (AOR, 1.9; P = 0.002) 和急诊科 (ED) 使用 (AOR, 2.8; P < 0.001)的概率明显增加。按疾病活动度分层后,单核细胞增多症患者到手术、住院和就诊的时间较短有关(P < 0.05)。
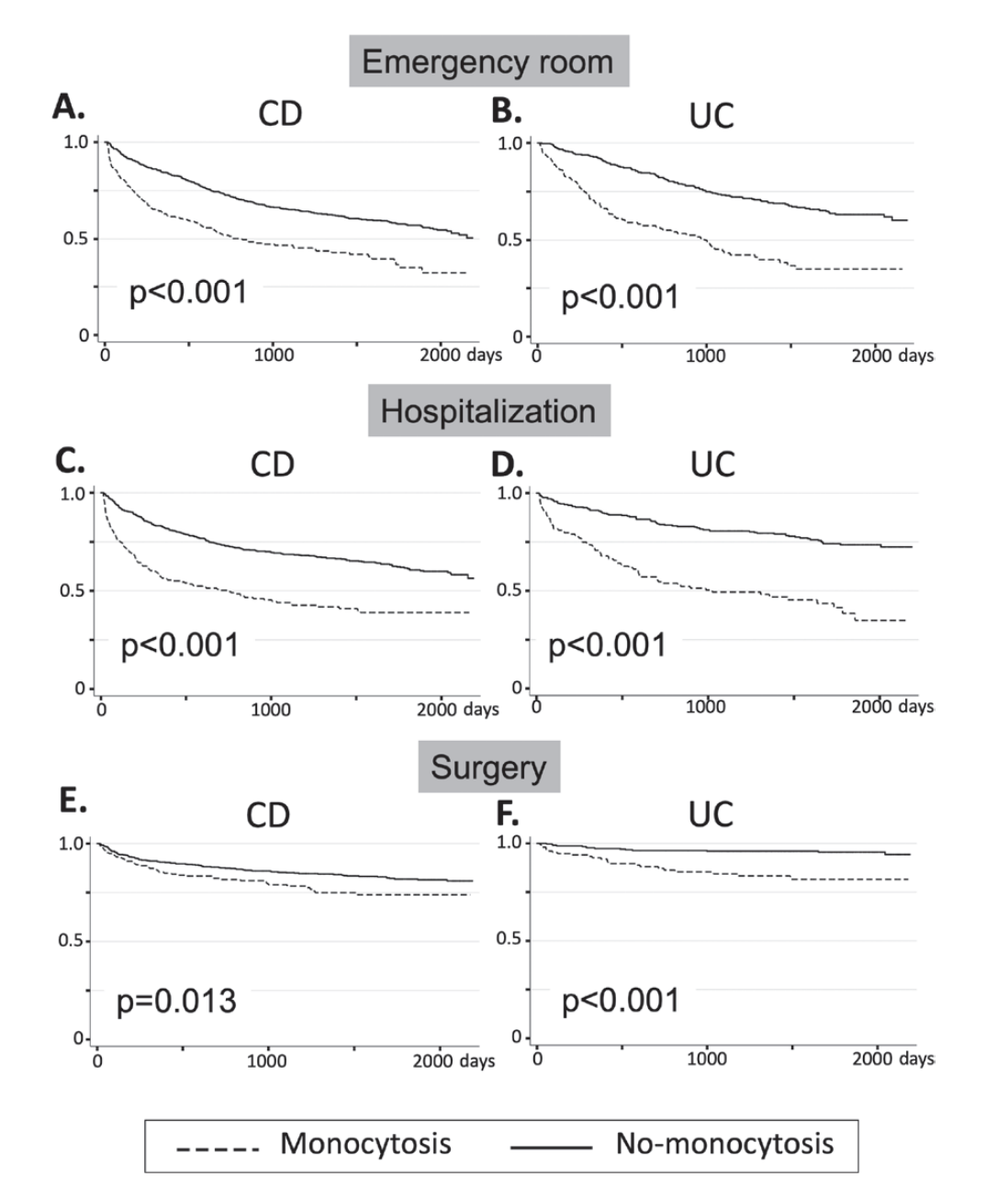
图:单核细胞增多症与炎症性肠病患者手术、住院的相关性
本项研究结果证实患有单核细胞增多症的 IBD 患者,无论疾病类型如何,都面临更差的临床结果、住院、手术和 ED 使用的风险。外周单核细胞增多症可能代表具有严重疾病的不同亚组的常规可用生物标志物
原始出处 :
Alyce Anderson. Et al. Monocytosis Is a Biomarker of Severity in Inflammatory Bowel Disease: Analysis of a 6-Year Prospective Natural History Registry. Inflammatory Bowel Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#标志物#
32
#IBD#
40
#单核细胞#
39
#炎症性#
28
#生物标志#
31
#生物标志#
34