JAMA:鼻插管高流量氧疗可降低重症新冠肺炎患者不良预后风险
2021-12-08 MedSci原创 MedSci原创
对于新冠肺炎重症患者,与常规氧疗相比,通过鼻插管高流量氧疗降低了机械通气风险,缩短了临床恢复时间。

Sars-cov-2感染导致的Covid-19病例通常是无症状或轻症的,但在大流行背景下,患者病情进展为急性低氧性呼吸衰竭的可能性大大增加,动脉低氧血症是重症Covid-19患者的主要特征,改善氧合是重要治疗手段,但机械通气患者的死亡率仍较高。无创呼吸支持可以限制肺损伤,同时预防与插管和机械通气相关的不良事件。近日研究人员考察了鼻插管高流量氧疗对Covid-19重症患者预后的影响。

研究在在哥伦比开展,共有220名成人因Covid-19住院,患者出现呼吸窘迫,动脉氧分/吸入氧分数比低于200,随机接受鼻插管高流量氧疗(n=109)或常规氧疗(n=111)。研究的主要终点为28天内气道插管需求以及临床痊愈。
220名随机患者中,199名被纳入终点分析(平均年龄60岁; 65名女性[32.7%])。高流量氧疗组34人(34.3%)插管,常规氧疗组51人(51.0%,危险比,0.62)。高流量氧疗组患者临床恢复的中位时间为11天,而常规氧疗组为14天(危险比,1.39)。 13名(13.1%)高流量氧疗组患者出现疑似细菌性肺炎,常规氧疗组17名(17.0%),分别有7名(7.1%)和11名(11.0%)患者出现菌血症。
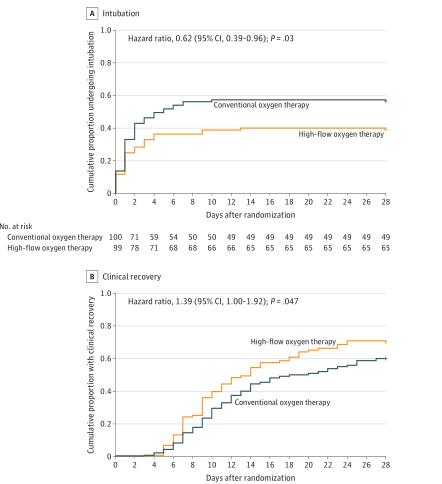
组间插管及康复时间差异
研究认为,对于新冠肺炎重症患者,与常规氧疗相比,通过鼻插管高流量氧疗降低了机械通气风险,缩短了临床恢复时间。
原始出处:
Gustavo A. Ospina-Tascón et al. Effect of High-Flow Oxygen Therapy vs Conventional Oxygen Therapy on Invasive Mechanical Ventilation and Clinical Recovery in Patients With Severe COVID-19 A Randomized Clinical Trial. JAMA. December 7,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#不良预后#
41
#氧疗#
56
#重症新冠肺炎#
54
学习了
45