JAMA:PERC、YEARS以及年龄调整D二聚体阈值联合用于急诊肺栓塞诊断
2021-12-08 MedSci原创 MedSci原创
对于急诊科疑似肺栓塞患者,与PERC联合D二聚体指标诊断方案相比,添加YEARS规则未显著降低后续血栓事件风险

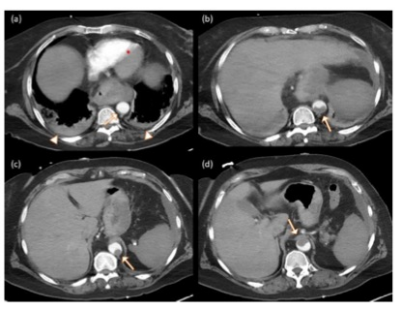
对于疑似肺栓塞(PE)患者的最佳诊断策略仍存在争议,传统的诊断根据D-二聚体测定和胸部影像学检查(CT肺血管造影术(CTPA)或肺通气/灌注[V/Q]扫描),但D-二聚体对PE的临床诊断特异性低,CTPA对PE的诊断率也仅在10%左右。研究人员开发了多种PE疑似患者排除方法,其中PERC规则(不满足以下全部条件可排除PE风险:年龄50岁以上、脉搏率≥100/min,动脉血氧饱和度<95%,单侧腿部肿胀、咯血、近期创伤或手术,既往PE或深静脉血栓史以及外源性雌激素的使用)或年龄调整的D-二聚体(50岁以上人群,D二聚体阈值为年龄×10 ng/mL)以及YEARS规则(3个标准:PE是最有可能的诊断、深静脉血栓形成临床症象和咯血,3条均无者,D-二聚体低于1000ng/mL可排除;满足1条以上者,D-二聚体低于500ng/mL可排除)。近日研究人员考察了PERC、YEARS规则以及年龄调整D-二聚体联合应用的临床价值。
本次研究在在法国和西班牙的18个急诊科(EDs)开展,为随机、交叉、非劣效性试验,总计1414名患者参与,存在至少1个PERC阳性指标,均不进行胸部成像,干预组包含726名患者,无YEARs阳性指标且D-二聚体水平低于1000 ng/mL或有1项YEARs阳性指标且D-二聚体水平低于年龄调整后阈值,则排除PE风险;对照组包含688名患者,若D-二聚体水平低于年龄调整后阈值则排除PE风险。研究的主要终点为3个月时静脉血栓栓塞(VTE),非劣效性边界为1.35%。次要终点包括胸部影像学异常、ED住院时间、住院时间、无指征抗凝治疗、全因死亡和3个月时全因再入院。
患者平均年龄55岁,女性占58%,1217名(86%)患者完成研究,其中100人急诊诊断为PE(7.1%)。3个月时,干预组1名患者出现VTE(0.15%),而对照组5名患者出现VTE(0.80%),调整后风险差异为-0.64%,满足非劣性终点。次要终点中,仅2项存在显著性差异,分别是胸部影像学异常(-8.7%)以及ED住院时间(-1.6小时),干预组表现出优势。
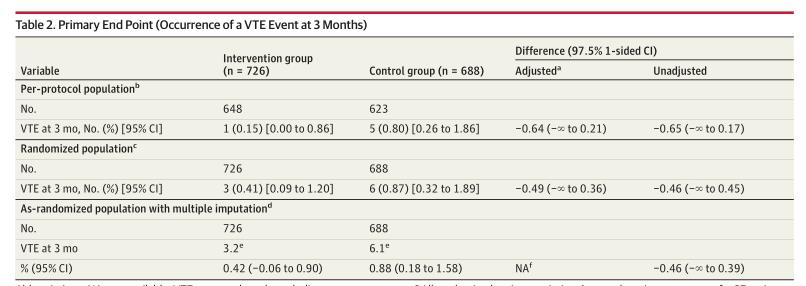
组间后续VTE风险差异不显著
研究认为,对于急诊科疑似肺栓塞患者,与PERC联合D二聚体指标诊断方案相比,添加YEARS规则未显著降低后续血栓事件风险。
原始出处:
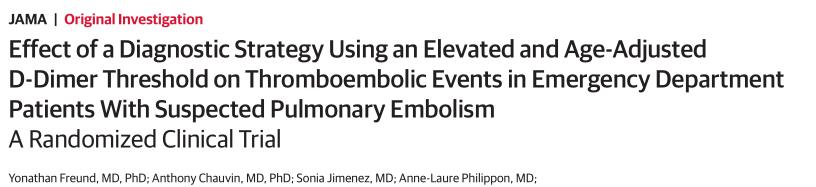
Yonathan Freund et al. Effect of a Diagnostic Strategy Using an Elevated and Age-Adjusted D-Dimer Threshold on Thromboembolic Events in Emergency Department Patients With Suspected Pulmonary Embolism A Randomized Clinical Trial. JAMA. December 7,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#二聚体#
35
#PE#
23
#阈值#
38
学习了
57