自身免疫性肝病诊断与处理,一文全讲解!
2022-01-28 消化界选自免E学苑 消化界选自免E学苑
自身免疫性肝病(AILD)尚处于初步研究阶段,发病机制尚不明确,其非特异性临床表现导致确诊困难,易造成漏诊、误诊,探究其发生机制有助于更好地指导AILD治疗。
自身免疫性肝病(AILD)主要包括自身免疫性肝炎(AIH)、原发性胆汁性胆管炎(PBC)和原发性硬化性胆管炎(PSC)。 AILD指机体产生的反应性细胞和抗体引起肝脏组织进行性不可逆损伤。约1/3的AILD患者伴肝外自身免疫性疾病,包括风湿病、内分泌病、胃肠道疾病、肺病、皮肤病。AILD的发病机制包括针对胆管细胞以及不同肝外组织的先天性和适应性免疫。AILD具有恶变倾向,可发展为肝癌,但进展相对缓慢。早期AILD对患者生活影响不明显,但疾病进展至晚期时,患者的生活质量较差,肝移植是AILD进展至终末期的唯一有效治疗方法。血清抗体检测对AILD的诊断有一定的辅助作用,但灵敏度和特异度均较低。此外多种补体也对AILD的诊断有一定价值。目前尚缺乏AILD的根治性治疗措施。现就近年关于AILD的发病机制和诊疗进展予以综述,以期为AILD治疗提供新方向。 AILD的发病机制 1 遗传因素 复杂的遗传结构是部分人群发生自身免疫性疾病的原因。AILD发病是多种基因相互作用的结果,对双胞胎家庭及群体研究结果表明,遗传作用在AILD发病风险中起重要作用。现已证实,人类白细胞抗原(HLA)单倍型与AILD遗传有关。研究表明,某些HLA等位基因与胆汁淤积性肝病有关,尤其是PBC中的HLA-DR8和PSC中的HLA-B*08。另外,在AIH中HLA单倍型DRB1*03-DRB1*04的存在与更具侵略性的疾病表型相关。HLA可反映免疫系统相关抗原的强度,但其与疾病的相关作用机制目前尚不清楚。全基因组关联研究和相关遗传研究进一步确定了遗传风险与AILD的联系,但潜在的功能影响仍有待证实。 2 环境因素 某些药物(如呋喃妥因、米诺环素)可以诱发AIH。药物诱发AIH的抗核抗体(ANA)/抗平滑肌抗体(SMA)的滴度相对较低。一般情况下,通过停药可使药物诱发的AIH达到临床缓解,但停药时间较长,往往需要数月甚至数年。药物诱发的AIH可能会发展为急性肝功能衰竭或慢性肝硬化,可能是药物代谢引起了免疫反应,导致肝毒性。 吸烟、使用激素替代疗法以及反复尿路感染病史与PBC的发展相关,PBC患者中复发尿路感染者较健康人更常见。ALID患者日常接触的物质(如指甲油、染发剂和清洁化学品)在PBC中起重要作用。 基于炎症性肠病(IBD)与PSC的关系,有学者提出微生物菌群变化可作为PBC的环境触发因素。感染也会增加AILD的患病风险,激活体内的免疫细胞,进而产生抗体攻击组织器官。 3 免疫因素 肝脏组织对自身免疫反应失去耐受性时,免疫细胞识别抗原的能力发生变化,导致免疫活化的T细胞持续攻击自身肝脏组织。AILD患者体内存在多种自身抗体,这些自身抗体是引起抗原抗体反应必不可少的媒介。唾液酸糖蛋白受体存在于肝脏组织中,并特异性表达于肝脏汇管区,这种蛋白受体的存在会引起自身的抗原抗体反应,破坏肝脏组织的自身免疫,从而造成肝细胞损伤,引起肝功能异常。抗线粒体抗体是PBC中较为重要的自身抗体。有研究报道,95%的PBC患者血清中可以检测到高滴度的抗线粒体抗体,往往在临床症状出现前便能检测到其高表达,抗线粒体抗体目前已成为诊断PBC的一项重要指标。ANA在80%的AIH患者血清中高表达;此外,SMA、抗肝胰抗体、抗肝/肾微粒体抗体等自身抗体在AILD进展中发挥重要作用。在免疫反应中,调节性T细胞与辅助性T细胞的数量和功能失衡是导致AILD患者免疫系统紊乱的关键因素。研究表明,体内趋化因子不仅诱导免疫细胞迁移,也调控免疫细胞的功能。 AILD的诊断 1 AIH的诊断 AIH确诊困难,典型AIH起病隐匿,大部分患者表现为慢性疾病急性发作,如疲劳、黄疸。疲劳、腹痛、黄疸和瘙痒等为非特异性临床表现,因此体格检查对确诊AIH无明显临床价值。肝功能检查丙氨酸转氨酶及天冬氨酸转氨酶升高,自身抗体ANA或SMA以及血清免疫球蛋白G水平升高是常见的AIH特征。ANA或SMA可在1型AIH患者体内检测到,除ANA和SMA外,有时AIH患者血清中亦可检测到抗肝/肾微粒体抗体,抗肝/肾微粒体抗体-1是2型AIH的特异性指标。但ANA和SMA并不是诊断AIH的特异性指标,在其他肝炎中也可检测到该类抗体。目前尚缺乏诊断AIH的高灵敏性和高特异性的生物标志物。AIH的确诊仍依赖病理活组织检查。组织学研究显示,AIH患者门静脉浆细胞增多,血浆淋巴细胞的改变与AIH活动程度显著相关。 2 PBC的诊断 PBC患者临床表现的差异较大。有50%~60%的PBC患者无症状或仅表现为肝功能异常。疲劳是PBC最常见的症状之一,80%的PBC患者存在疲劳症状,但疲劳与疾病严重程度或持续时间无关。PBC常见的皮肤表现包括色素沉着、黄疸、黄瘤、皮肤干燥等。部分PBC患者因肝硬化并发症(如曲张静脉出血、黄疸、腹水以及肝性脑病)就诊。黄疸继发于胆汁淤积,20%~70%的PBC患者出现瘙痒症状,这是残留胆汁盐的皮肤神经作用。夜间、高温及妊娠期间瘙痒症状加重,影响20%~70%的PBC患者。40%~65%的PBC患者还可合并其他风湿病或自身免疫性疾病,以干燥综合征和自身免疫性甲状腺疾病最常见。 PBC患者也可合并皮肤硬皮病,5%~10%的患者可伴有类风湿关节炎。终末期PBC患者可能出现门静脉高压。实验室检查显示,抗线粒体抗体诊断PBC的特异性较高,尤其是抗线粒体抗体M2型,只表达于胆管上皮细胞。PBC应与胆道梗阻/狭窄、PSC、药物性肝病等相鉴别。 3 PSC的诊断 约50%的PSC患者无症状,仅在体格检查或因IBD检查时发现胆汁淤积指标升高而确诊。现有PSC诊断治疗指南指出,除外其他胆汁淤积的原因,通过典型影像学表现即可确诊。胆汁淤积是PSC的主要病因,血清碱性磷酸酶升高是PSC的特异性改变。除此之外,PSC患者的总免疫球蛋白水平升高(免疫球蛋白M为50%),抗中性粒细胞胞质抗体阳性。磁共振胰胆管造影是目前较常用的诊断PSC的影像学检查,灵敏度为86%,特异度为94%。PSC患者罹患肝胆和大肠癌的风险显著增加,尤其是PSC合并克罗恩病者。PSC应与继发性硬化性胆管炎、组织细胞增生症、胆管狭窄、PBC等疾病鉴别。 AILD的治疗 1 AIH的治疗 AIH治疗的总体目标是诱导并维持炎症的完全抑制,防止疾病进展为肝硬化和肝功能不全。免疫抑制治疗是AIH的一线治疗方法,包括皮质类固醇或皮质类固醇联合硫唑嘌呤。美国肝病研究协会建议使用泼尼松单药(60mg/d)或泼尼松(30mg/d)联合硫唑嘌呤(50mg/d)治疗。一项回顾性调查研究表明,泼尼松初始剂量较高或较低不影响转氨酶的正常化率,提示泼尼松的使用剂量较先前假设的剂量低。AIH的治疗可分为诱导阶段和维持阶段,当患者临床症状消失,转氨酶和免疫球蛋白达到正常水平时,提示AIH缓解。AIH的标准诱导疗法包括高剂量泼尼松或泼尼松联合硫唑嘌呤治疗。应用泼尼松的不良反应明显,与泼尼松相比,布地奈德的不良反应较少。布地奈德的肝脏首过效应较明显,首过清除率约90%,不良反应不明显,布地奈德联合硫唑嘌呤缓解非肝硬化性AIH患者症状的效果较泼尼松更佳。但布地奈德对AIH患者合并肝硬化患者无效。AIH症状完全缓解后,治疗周期通常持续2年左右。AIH的二线替代治疗药物为霉酚酸酯,霉酚酸酯通过抑制肌苷磷酸脱氢酶抑制鸟嘌呤核苷酸的合成,最终使DNA合成受阻。回顾性研究显示,霉酚酸酯治疗对类固醇皮质激素反应不足或不耐受的AIH有效,且耐受性良好。专家推荐的AIH二线治疗药物包括钙调神经磷酸酶抑制剂(环孢菌素A和他克莫司)、雷帕霉素靶蛋白抑制剂(西罗莫司和依维莫司)、生物制剂、熊去氧胆酸等。B细胞消耗是一种极具应用前景的AIH治疗方法,VAY736是B细胞激活因子受体阻断剂,临床试验显示出较好的治疗效果,且无严重副作用。 免疫抑制疗法对肝移植术后AIH的效果甚微。针对复发性AIH,重新使用皮质类固醇和硫唑嘌呤或提高药物剂量可能有效。难治性AIH患者可以选择环孢菌素、西罗莫司或霉酚酸酯治疗。 2 PBC的治疗 熊去氧胆酸是治疗PBC的首选药物,可改善胆汁酸代谢。熊去氧胆酸可促进胆汁循环,增加胆汁分泌,还可以调节免疫功能,且不良反应较少,能够延缓PBC病情进展。有研究表明,与未经熊去氧胆酸治疗的PBC患者相比,经熊去氧胆酸治疗PBC患者的肝功能血清指标(如丙氨酸转氨酶、天冬氨酸转氨酶、γ谷氨酰胺转肽酶、总胆红素)显著下降。此外,熊去氧胆酸还可以调节PBC患者的肠道菌群,改善脑血管活性。 免疫抑制剂对于PBC也有一定的治疗作用。研究表明,布地奈德可调节肝脏各种代谢酶的活性,延缓组织学进展。因此推荐布地奈德作为PBC的二线治疗药物。有研究发现,贝特类药物联合熊去氧胆酸对PBC早期患者有效,且不良反应发生率低。 我国传统医学将PBC归属于“虚劳”“胁痛”“黄疸”“积聚”“鼓胀”等的范畴,运用辨证施治以四君子汤为基础药方,方选黄芪四君子汤合柴胡疏肝散进行健脾疏肝治疗有一定的效果。 3 PSC的治疗 目前PSC的治疗尚不确定。虽不推荐熊去氧胆酸用于PSC的治疗,但其能刺激胆汁酸分泌,在实际临床工作中已被作为PSC的治疗药物。目前熊去氧胆酸治疗PSC的剂量不超过28mg/(kg·d)。奥贝胆酸(5~10mg)治疗可显著降低PSC患者血清中碱性磷酸酶的水平。泼尼松、布地奈德、秋水仙碱、青霉素、硫唑嘌呤、他克莫司、甲氨蝶呤、霉酚酸酯均对PSC有一定的益处。胆囊息肉>8mm是PSC患者行胆囊切除术的指征。对于因明显胆管狭窄而接受经内镜逆行胰胆管造影治疗的PSC患者,必须对可疑狭窄部位胆管进行病理活组织检查。使用经内镜逆行胰胆管造影球囊扩张缓解症状时,单纯胆管扩张效果较胆道支架置入好。考来烯胺(或类似药物)是治疗PSC伴瘙痒症状的一线药物,利福平和纳曲酮是二线治疗药物,肝移植是治疗PSC最有效的方法。 AILD严重威胁人类的生命健康,导致患者生活质量严重下降以及心理和精神压力增加。目前尚无AILD的根治性治疗方法,皮质类固醇和硫唑嘌呤是目前治疗AIH的一线药物,霉酚酸酯是二线治疗药物。PSC亦缺乏有效的治疗方案,熊去氧胆酸、激素类药物以及免疫抑制剂对PBC可能有一定的治疗效果,但缺乏研究支持,肝移植是终末期PSC患者的有效治疗方法。 AILD尚处于初步研究阶段,发病机制尚不明确,其非特异性临床表现导致确诊困难,易造成漏诊、误诊,探究其发生机制有助于更好地指导AILD治疗。通过高新技术及基因组学研究探索AILD的发病机制、早期标志物、治疗靶点可能是未来AILD研究的方向。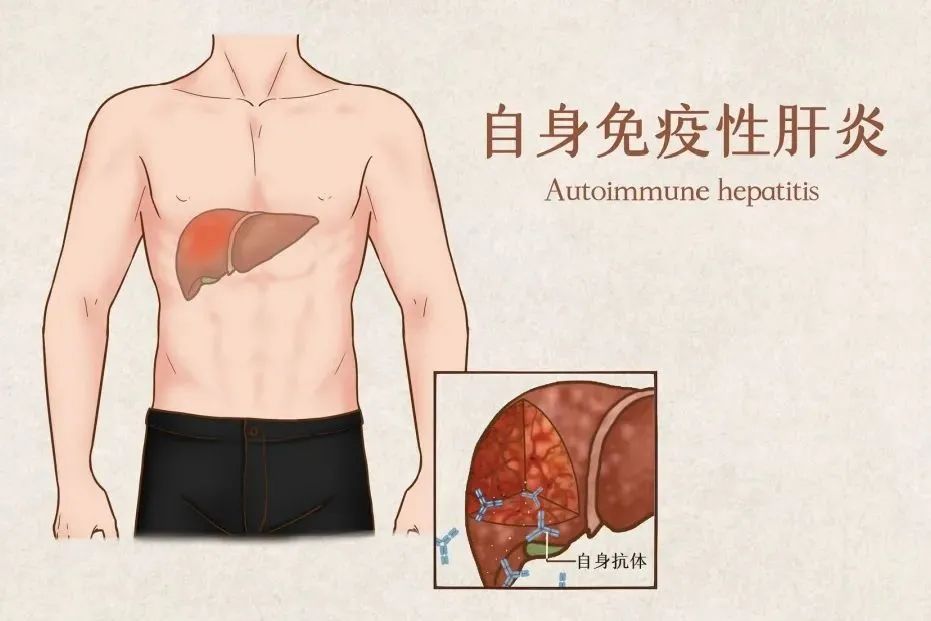

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了
55
学习
0
学习
53
#自身免疫性肝病#
43
学习了
68
学习了
61
其理论上的肠道选择性可能会降低肠
60
学习了学习了
0