Br J Cancer:LIMCH1和HLA-DQB1为侵袭性宫颈癌的潜在标志物
2021-03-23 xiaozeng MedSci原创
宫颈癌是全球女性中的第四大癌症类型,且造成每年超过311,000名患者致命。大多数的癌症相关死亡与该疾病一级治疗后出现的肿瘤转移或疾病的复发相关。
宫颈癌是全球女性中的第四大癌症类型,且造成每年超过311,000名患者致命。大多数的癌症相关死亡与该疾病一级治疗后出现的肿瘤转移或疾病的复发相关。
在宫颈癌中,90%的疾病复发发生于最初诊断的3年内,其中不到5%的患者存活超过5年。由于晚期宫颈癌的预后极差,几乎没有治疗选择。因此,鉴定有效的分子标志物对于改善患者的个性化治疗至关重要。
该研究旨在调查与患者生存和复发相关的宫颈癌转录数据,以确定潜在的侵略性疾病驱动因子。
研究人员通过比较20例复发患者和53例治愈患者原发性肿瘤的RNA测序数据,并通过免疫组化确定所选标志物的蛋白水平和预后影响。
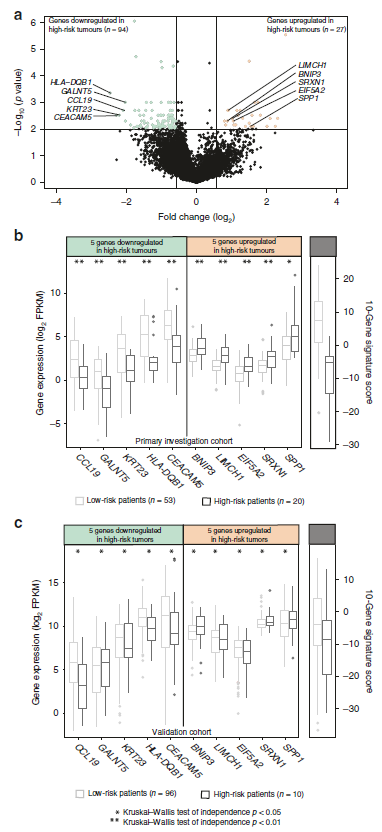
预后特征的识别
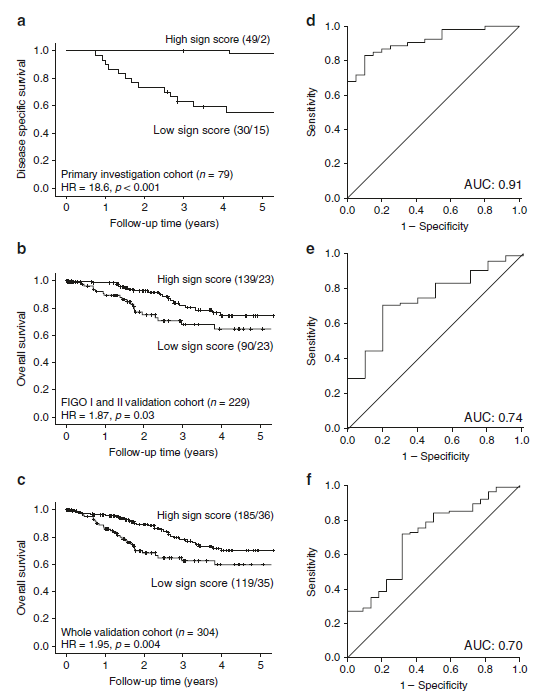
结果显示,根据患者的疾病复发状态,研究人员发现了121个差异表达的基因,从中鉴定出了具有高预后意义的10个标志物,并在一个独立的患者队列中进行了验证。
当对已建立的预后指标进行调整后,研究人员发现,HLA-DQB1和LIMCH1这两个标志基因的蛋白水平是患者存活的独立预测因素(HLA-DQB1的风险比为2.50,而LIMCH1为3.19)。HLA-DQB1的蛋白表达水平与PD-L1(程序性死亡配体1)阳性状态相关。基因富集分析显示,HLA-DQB1高表达水平的肿瘤伴随着IFN-γ(干扰素-γ)的免疫激活和响应。
10个基因标志物的预后影响
总而言之,该研究结果揭示了在宫颈癌中具有高预后能力的10个基因标志物。其中HLA-DQB1和LIMCH1或可成为指导宫颈癌治疗的潜在生物标志物。
原始出处:
Halle, M.K., S?dal, M., Forsse, D. et al. A 10-gene prognostic signature points to LIMCH1 and HLA-DQB1 as important players in aggressive cervical cancer disease. Br J Cancer (15 March 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#标志物#
46
#侵袭性#
47
#宫颈#
49
#HLA#
49