Nat Cancer:新辅助治疗药物卡博替尼和纳武单抗治疗局部晚期肝细胞癌
2021-08-02 xiaozeng MedSci原创
肝细胞癌(HCC)占所有原发性肝癌的90%以上,该疾病通常由慢性肝病发展的,包括酒精性肝病、慢性病毒性肝炎(乙型或丙型)以及非酒精性脂肪肝病。
肝细胞癌(HCC)占所有原发性肝癌的90%以上,该疾病通常由慢性肝病发展的,包括酒精性肝病、慢性病毒性肝炎(乙型或丙型)以及非酒精性脂肪肝病。
HCC作为癌症相关死亡的第四大原因,在美国和全球许多地区其死亡率逐年上升。潜在的治愈性肝切除术是HCC的最佳治疗方法,但大多数的患者并不适合切除术治疗,且大多数进行切除的HCC患者最终会出现疾病的复发。
由于在手术切除时通常会观察到阴性的切缘,所以认为HCC的复发通常是由切除后持续存在的微转移所引起的。因此,可减少微转移疾病负担的围手术期治疗策略或可能改善患者的预后。
既往研究显示,对于某些癌症,新辅助治疗策略可减少肿瘤的体积,使得局部晚期或无法进行切除手术的癌症患者获得二次可切除性。然而,HCC患者的新辅助全身治疗策略一直受到缺乏有效得全身药物治疗的限制,且目前并无相关的系统疗法被批准用于HCC的新辅助治疗。
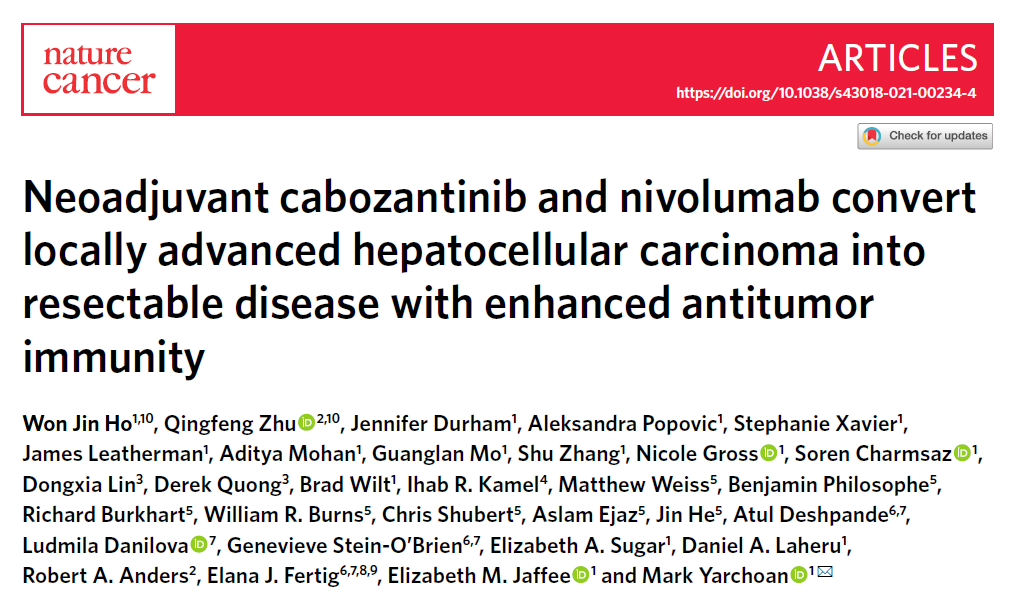
新辅助药物卡博替尼和纳武单抗的临床反应
该研究为一项单臂1b期临床试验,在该研究中,研究人员旨在评估新辅助药物卡博替尼(cabozantinib)和纳武单抗(nivolumab)在HCC患者中的可行性,包括了传统切除标准之外的患者。
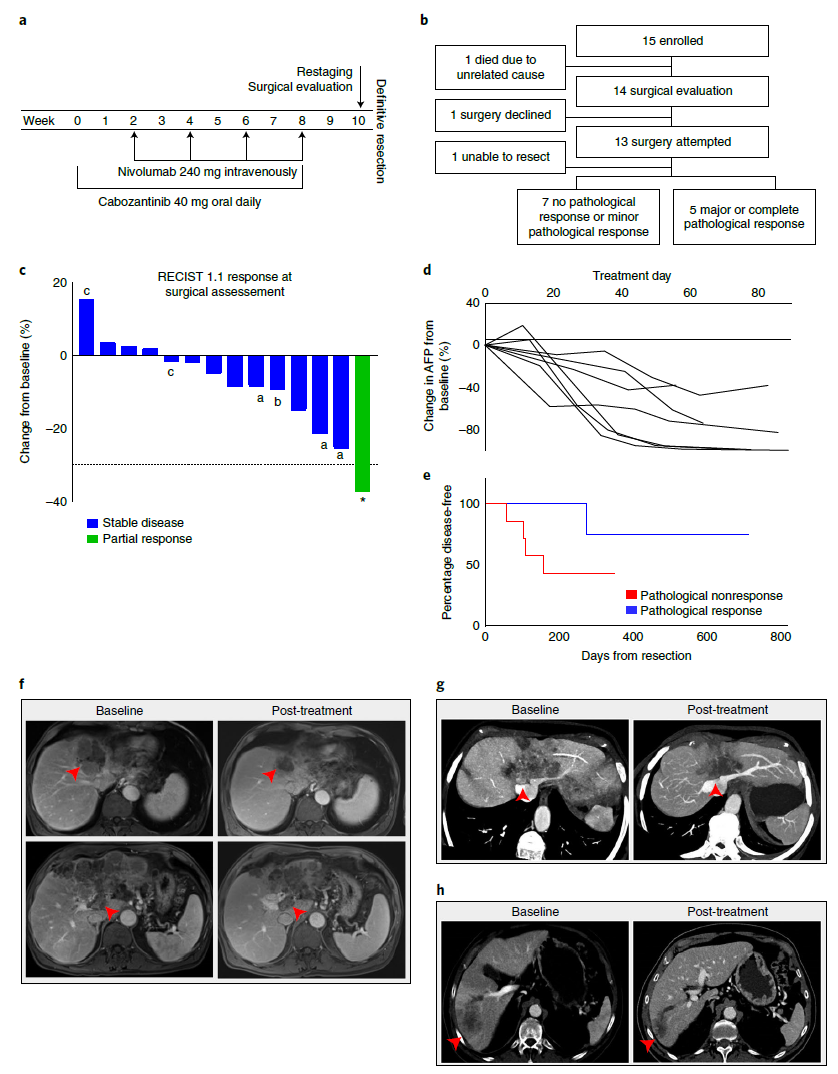
结果显示,在入组的15名患者中,12名患者(80%)成功进行了切除术且切缘阴性,12名患者中有5名(42%)出现了严重的病理反应。生物样本分析显示,相比于无反应者,出现反应得患者的效应T细胞、三级淋巴结构、CD138+浆细胞和B细胞的空间排列明显丰富了,说明B细胞贡献于HCC的抗肿瘤免疫。
卡博替尼可增强全身和局部抗肿瘤T细胞反应
总而言之,该研究结果揭示,卡博替尼和纳武单抗作为一种合理的治疗组合,可用于测试新辅助治疗对可切除或局部晚期HCC的效用。
原始出处:
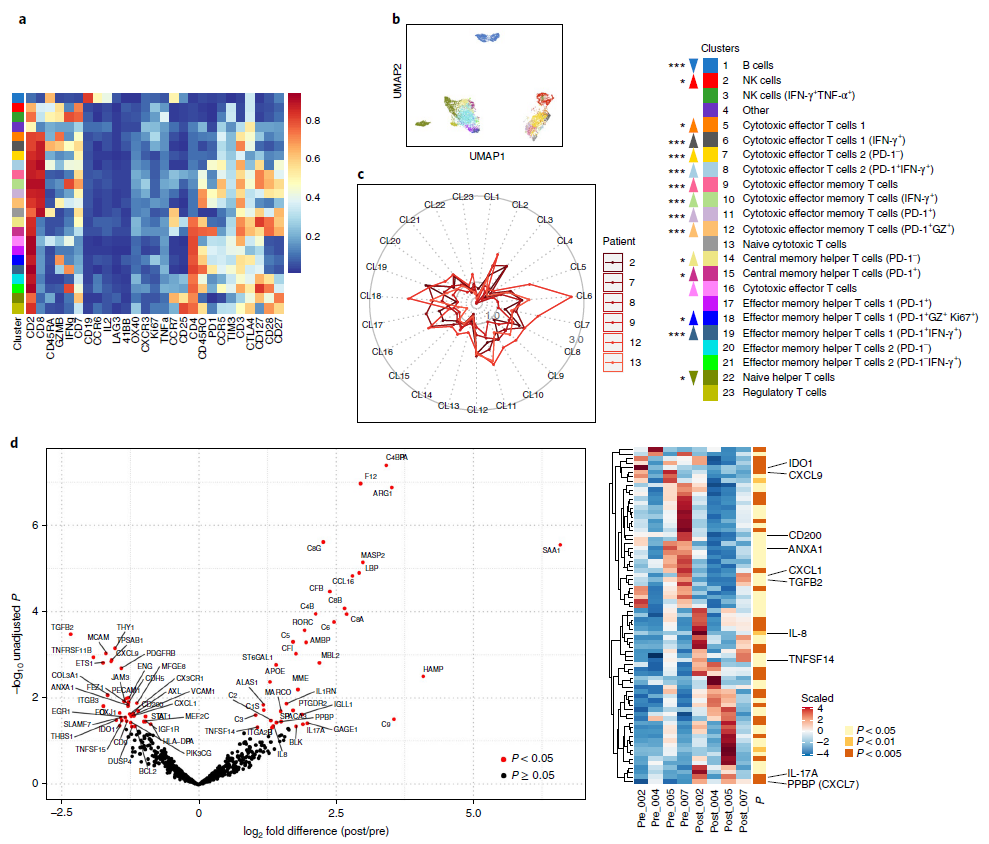
Ho, W.J., Zhu, Q., Durham, J. et al. Neoadjuvant cabozantinib and nivolumab convert locally advanced hepatocellular carcinoma into resectable disease with enhanced antitumor immunity. Nat Cancer (29 July 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#细胞癌#
41
#新辅助#
36
#Nat#
34
#局部晚期#
29
#肝细胞#
27
#治疗药物#
25
#晚期肝细胞癌#
29
#局部#
37