Front Oncol:顺铂联合伊立替康一线治疗转移性或不能切除的胸腺癌疗效显著耐受性好
2022-01-16 yd2015 MedSci原创
研究表明,顺铂联合伊立替康作为转移性胸腺癌的一线化疗方案疗效显著,且毒性可接受。
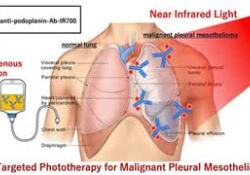
以铂为基础的化疗是转移性或不能切除的胸腺癌的标准治疗方法。但是,最佳的化疗方案尚未确定,包括是否应与二线或以上标准抗肿瘤药物联合使用。因此,来自日本的团队开展了回顾性研究,评估顺铂联合伊立替康一线治疗转移性或不能切除的胸腺癌的疗效和安全性。相关结果发表在Frontiers in Oncology杂志上。
该研究主要终点为ORR。次要终点为疾病控制率(DCR)、无进展生存期(PFS)、总生存期(OS)和毒性(不良事件)。
18例既往未经治疗的转移性/不可切除胸腺癌患者接受了伊立替康和顺铂治疗。7例(39%)ECOG PS为0,11例(61%)ECOG PS为1。3例患者(17%)为 Masaoka-Koga IVa期,15例(83%)为IVb期。最常见的转移部位是肺。在病理诊断方面,鳞状细胞癌14例(77%),未分化癌3例(17%),大细胞神经内分泌癌1例(6%)。
联合治疗的ORR为 44% ,DCR为89%,其中 8例(44%)获得PR,8例(44%) 为SD。
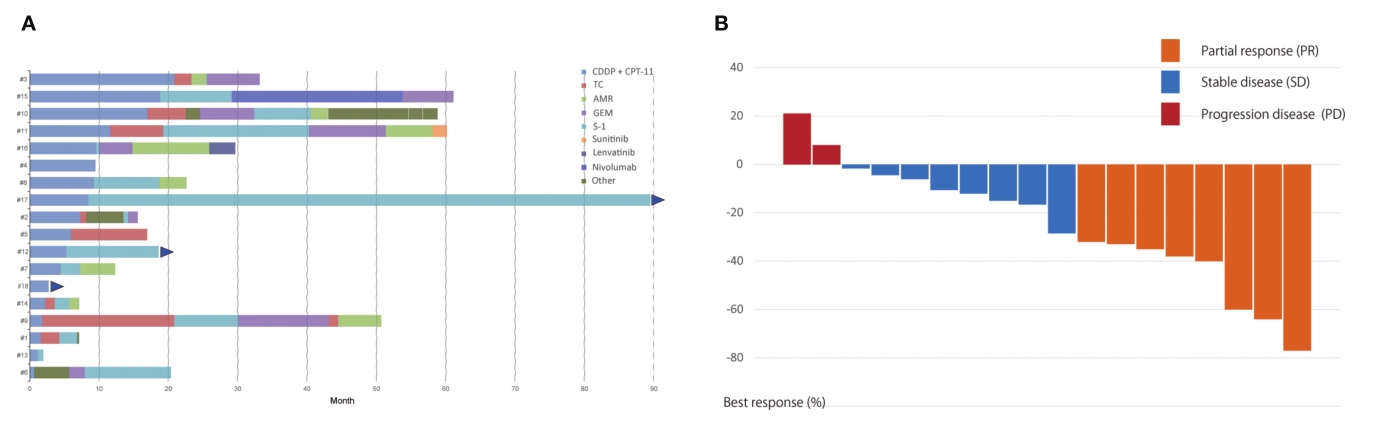
疗效评估
中位随访时间29.5个月,中位无进展生存期(PFS)为8.4个月[95%CI: 2.7-11.6个月]。中位OS为45.6个月(95% CI: 15.7-69.1个月)。
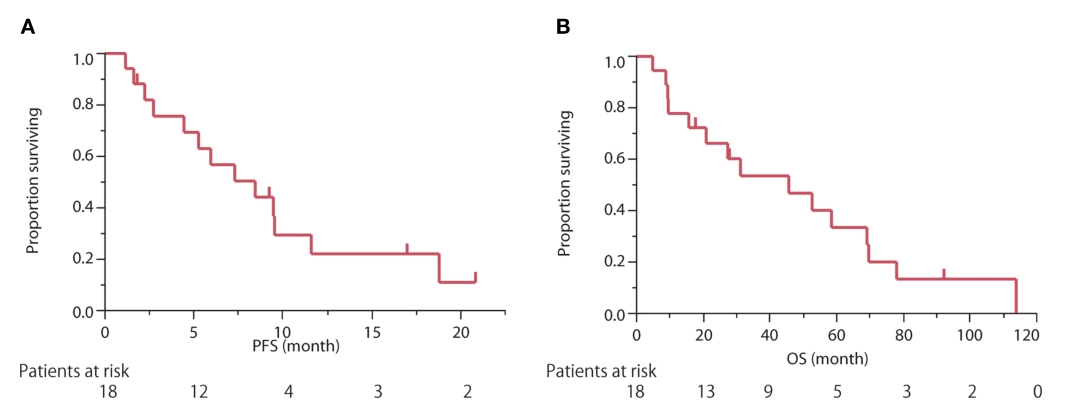
PFS和OS
15名患者接受了S-1为二线或后线治疗方案,ORR为33%,中位无进展生存期为8.1个月(95% CI: 0.7-10.3个月)。8例患者接受卡铂和紫杉醇作为二线或后线治疗方案,ORR为38%,中位无进展生存期为4.1个月(95% CI: 0.9-7.7个月)。1名患者接受了nivolumab作为三线治疗方案,无进展生存期为25个月。1名患者接受了仑伐替尼作为第五线化疗,PFS为3.4个月。
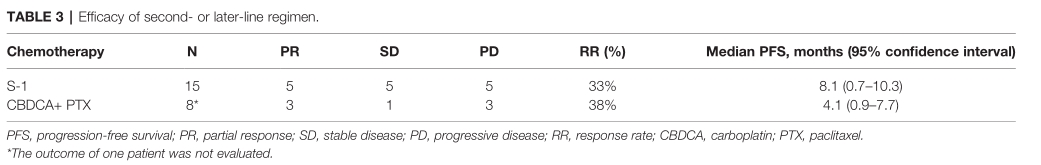
二线或后线治疗的疗效
6例患者出现3级血液毒性。主要治疗相关不良事件为恶心(73%)、中性粒细胞减少(72%)和白细胞减少(45%)。3例出现3级中性粒细胞减少;然而,没有一例患者出现发热性中性粒细胞减少。5例患者出现3级非血液学不良事件,1例患者出现3级腹泻。无患者出现4级不良事件,无治疗相关死亡。3例患者因胃肠道不良事件停用顺铂和伊立替康方案。
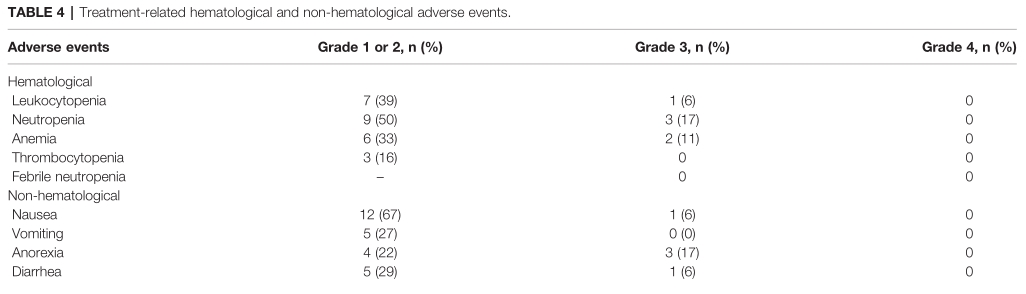
AEs
综上,研究表明,顺铂联合伊立替康作为转移性胸腺癌的一线化疗方案疗效显著,且毒性可接受。
原始出处:
Fukuda A, Okuma Y, Hakosaki T, Mirokuji K, Yomota M, Hishima T and Hosomi Y (2022) Cisplatin and Irinotecan as First-Line Chemotherapy for Previously Untreated Metastatic Thymic Carcinoma: Updated Analysis. Front. Oncol. 11:779700. doi: 10.3389/fonc.2021.779700
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
55
#胸腺#
40
#铂#
56
#胸腺癌#
47
#转移性#
39
#耐受性#
50
学习了,谢谢分享
69