Clin Gastroenterology H:普雷米司特(磷酸二酯酶-4的口服抑制剂)在活动性溃疡性结肠炎患者中的疗效分析
2020-10-14 MedSci原创 MedSci原创
溃疡性结肠炎(UC)是影响结肠的一种慢性复发性炎症,目前尚无治愈方法。当前的治疗方法包括非生物药物(美沙拉敏,皮质类固醇,免疫抑制剂。)
溃疡性结肠炎(UC)是影响结肠的一种慢性复发性炎症,目前尚无治愈方法。当前的治疗方法包括非生物药物(美沙拉敏,皮质类固醇,免疫抑制剂),生物药物(英夫利昔单抗,阿达木单抗,戈利木单抗,维多珠单抗)和口服免疫调节剂(托法替尼)。许多患者对这些疗法会出现无反应或不耐受的现象,UC患者需要特异性、耐受性更好的药物,口服小分子磷酸二酯酶4(PDE4)抑制剂普雷米司特(Apremilast)在细胞内起作用以调节炎症的作用。因此可能可以用于UC的治疗,本项研究对常规疗法无反应或不耐受的溃疡性结肠炎(UC)患者接受普雷米司特后的效果进行了探究。

研究人员对患有活动性UC的成年患者进行了为期3个月或更长时间的双盲,2期临床药物试验,这些成年人从未接受过生物疗法,或者因传统疗法而失败,不能耐受或有禁忌症而纳入本项研究。患者被随机分为两组,接受每天两次,分别服用普瑞司特30 mg(n = 57),普瑞司特40 mg(n = 55)或安慰剂(n = 58),连续12周的治疗;然后将患者随机分为每天两次接受30或40毫克普瑞司特的组,再持续40周。并在第12周和第52周进行内窥镜检查并收集活检。主要观察终点是第12周的临床缓解情况。
研究结果显示:30 mg普雷司特组在第12周时达到临床缓解的患者为31.6%,在安慰剂组中为12.1%(P = .01)。但是,在40 mg普雷司特组中,只有21.8%的患者在第12周达到了临床缓解(P= 0.27)。30 mg和40 mg的普雷司特组之间的临床缓解差异与内镜改善的差异相关。两组普雷司特组的Mayo评分成分(大便频率评分,直肠出血评分,医生的整体评估)均较基线有相似的改善。与安慰剂组相比,在30周和40 mg的普雷司特组中,到第12周时,C反应蛋白和粪便钙卫蛋白的中位数降低百分比更高。在第52周时,最初分配给普雷司特30 mg组的患者中有40.4%的患者达到临床缓解,最初分配给普雷司特40 mg组的患者中有32.7%的患者达到了临床缓解。
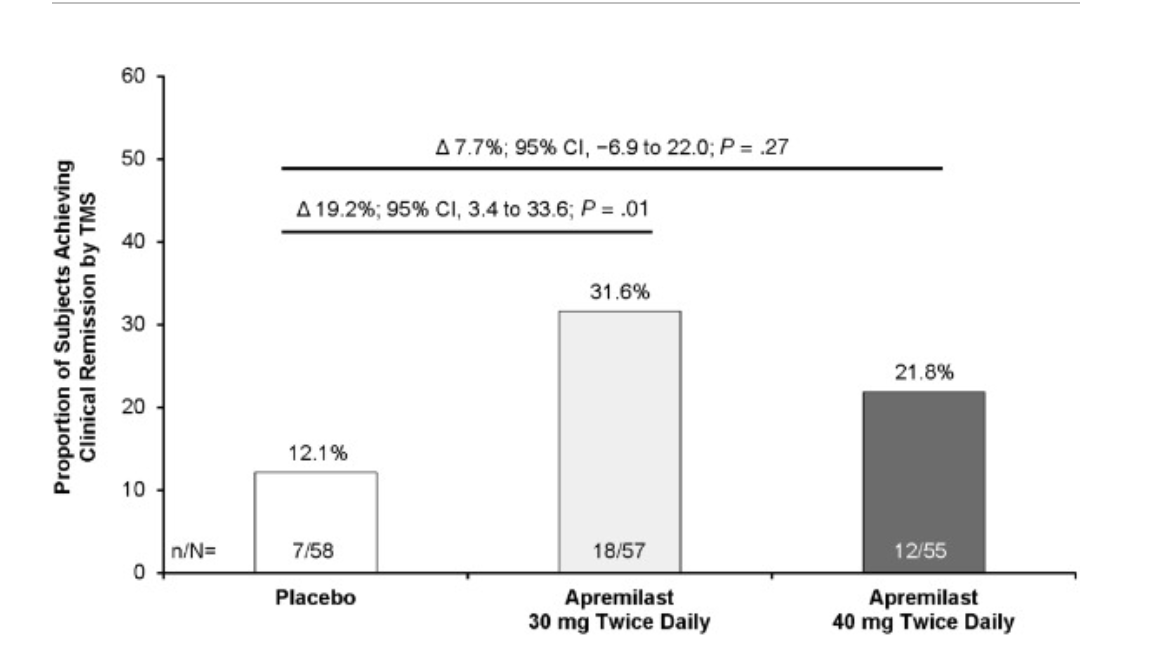
最后研究人员说道:接受30毫克或40毫克普雷司特治疗的活动性UC患者中,临床和内窥镜检查以及炎症指标均可以得到明显改善。
原始出处:
Silvio Danese. Et al. Effects of Apremilast, an Oral Inhibitor of Phosphodiesterase 4, in a Randomized Trial of Patients With Active Ulcerative Colitis. Clinical Gastroenterology and Hepatology.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#活动性溃疡性结肠炎#
33
#疗效分析#
33
#Gastroenterol#
38
#GAS#
33
#活动性#
34
#AST#
35
#抑制剂#
32
#口服抑制剂#
36
#溃疡性#
36
#Gastroenterology#
27