JAHA:老年女性久坐行为与心房颤动的关系
2022-03-08 MedSci原创 MedSci原创
在这项针对居住在社区的老年女性的前瞻性研究中,总久坐时间和久坐久坐模式与较高的心房颤动风险相关,但这些关联因身体机能和自我报告的健康状况的调整而有所减弱。
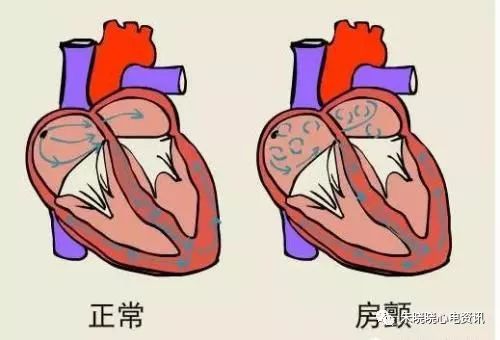
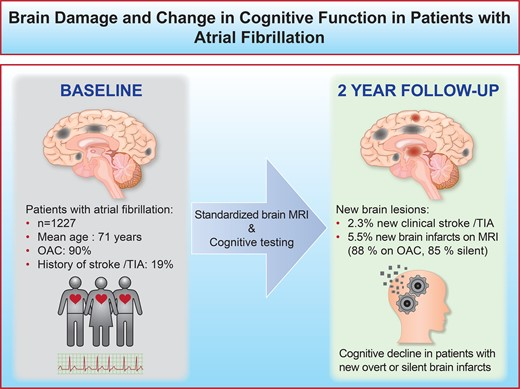
心房颤动是美国最常见的心律失常,是卒中和死亡率的独立预测因子。久坐行为与心血管疾病相关,但其与心房颤动之间的相关性尚未得到很好的研究。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员的目的是评估客观测量的久坐行为与心房颤动事件之间的关联。

研究人员通过佩戴在腰带上1周的三轴加速度计测量了受试者的久坐行为。心房颤动事件是从医疗保险索赔中确定的。研究人员使用针对人口统计学和临床协变量调整的Cox比例风险模型评估了总久坐时间(或久坐行为模式)与心房颤动事件之间的关联。

在2675名参与者(平均年龄为78.2岁)中,有268名(10.0%)受试者发生心房颤动,发病率为每1000人每年31例。在调整年龄、种族和民族、体重指数、教育、吸烟史、高血压、糖尿病、卒中、心脏病和其他慢性病后,更长的总久坐时间与更高的心房颤动风险相关(第4四分位数与第1四分位数相比的风险比为1.20,[95%CI为0.81-1.78];趋势P=0.05)。在调整身体机能和自评健康后,这一相关性不再具有统计学意义。更长的平均久坐时间和更连续的久坐时间(相对于久坐时间的频繁休息)也与更高的心房颤动风险相关,但这些关联也随着连续调整而有所减弱。
在这项针对居住在社区的老年女性的前瞻性研究中,总久坐时间和久坐久坐模式与较高的心房颤动风险相关,但这些关联因身体机能和自我报告的健康状况的调整而有所减弱。这表明久坐行为与心房颤动之间的关联可能归因于对整体功能和健康。
原始出处:
Brian C. Boursiquot.et al.Sedentary Behavior and Atrial Fibrillation in Older Women: The OPACH Study.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.023833
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#AHA#
37
#心房#
52
好
51
好文章,值得一读。
53