JAMA Neurology:心脏和非心脏大手术中Tau和神经退行性变的血浆生物标志物
2021-11-15 Naomi MedSci原创
神经细胞损伤的血浆生物标志物,包括总tau和神经丝轻链(NFL),提示手术可以触发损伤。该研究证实了先前报道的大手术患者总tau和NFL水平升高,并证明血浆pTau181平行增加。
大手术往往合并术后神经认知障碍。受影响的患者表现出记忆和执行功能问题,类似于阿尔茨海默病(AD)中的缺陷。一个关键问题是,手术是否可加剧或揭露潜在的阿尔茨海默病(AD)发展的病理生理。
神经细胞损伤的血浆生物标志物,包括总tau和神经丝轻链(NFL),提示手术可以触发损伤。与不同脑部疾病中总tau和NFL水平升高不同,在苏氨酸残基181处磷酸化的tau蛋白水平(PTau181)是相对特异的,并可预测AD。但大手术是否触发血浆pTau181增加尚不清楚。近日,有研究人员对接受心脏手术/髋关节置换手术的患者围绕手术时间测定的总Tau、NFL、PTau181进行了追踪与对比。
这项研究得到了斯坦福大学机构审查委员会的批准。所有参与者都给予书面知情同意。研究对象为需要体外循环的心脏手术患者(n=6)和髋关节置换手术患者(n=8)。心内直视手术患者分别于麻醉诱导前、麻醉诱导后、切开后、体外循环时、体外循环结束后、术后第1天和第2天采血(6例中仅4例于诱导前和术后第2天采血),分别于麻醉诱导前、麻醉诱导后、体外循环结束后、术后第1天和第2天采血。在接受髋关节置换手术的患者中,分别在手术前、术后1小时以及术后第1天和第2天采血。对每个样本的pTau181、总tau和NFL血浆浓度进行了分析(附录中的eMethods)。重复测量方差分析和Tukey后检验检验了时间变化(调整后P<0.05)。
- 5名男性和1名女性接受心脏手术,平均年龄65岁(范围53-83岁)。5名男性和3名女性接受了髋关节置换手术,平均年龄76岁(范围33-84岁)。
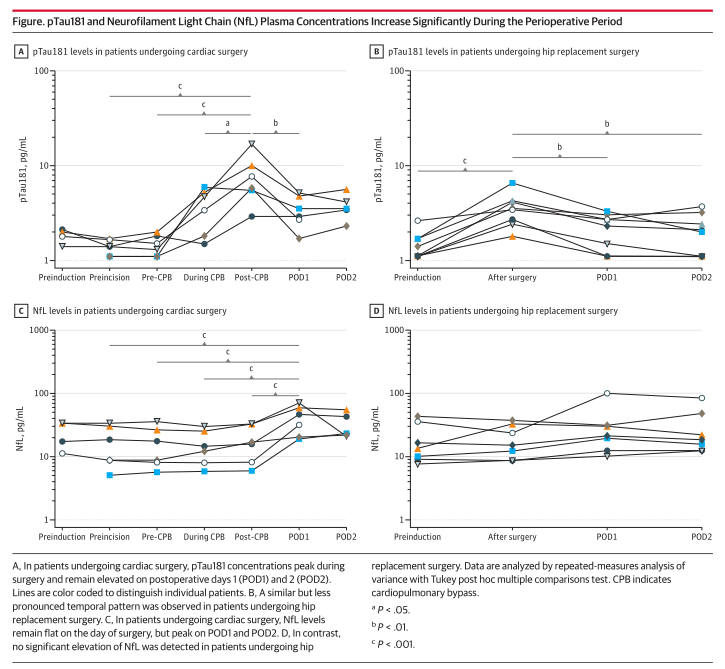
- 在接受心脏手术的患者中,术前血浆pTau181浓度的中位数为1.40pg/mL(范围为1.10-1.66),低于阈值(1.81pg/mL),与进展到AD有关。术中,pTau181浓度增加5.1倍至6.75pg/mL(范围为2.90-17.20)(图A)。血浆总tau水平增加了26.1倍,从2.44pg/mL(范围为1.58-4.12)增加到58.74pg/mL(范围为3.43-92.60)(数据可从I.F.索取)。PTau181和总tau水平在POD1和POD2仍然较高,但不显著。
- 在接受髋关节置换手术的患者中,pTau181水平在手术后立即从1.25pg/mL(范围为1.10-2.60)增加到3.45pg/mL(范围为1.806.50),增加了2.5倍(图B)。总tau水平增加了3.8倍,从2.05pg/mL(范围为0.90-3.66)增加到9.47pg/mL(范围为2.24-16.1)(数据可从I.F.索取)。PTau181和总tau水平在POD1和POD2仍然较高,但不显著。
- 在接受心脏手术的患者中,血浆NFL在手术过程中保持不变,但在POD1时上升了2.4倍,从13.69pg/mL(5.02-33.90)上升到39.40pg/mL(19.10-71.40),POD2仍然升高(图C)。
- 在接受髋关节置换手术的患者中,NFL水平在手术过程中也没有变化,但在POD1中增加了1.4倍,从13.5pg/mL(范围为7.45-42.40)上升到21.0pg/mL(范围为10.1099.60),并在POD2保持升高,尽管没有显著差异(图D)。
结果证实了先前报道的大手术患者总tau和NFL水平升高,并通过证明血浆pTau181平行增加。
Tau的过度磷酸化与其加速从微管分离并聚集成神经纤维缠结有关,尽管这些变化与神经元功能障碍和死亡的关系仍在积极研究中。血浆中磷酸化的tau亚型水平升高,包括pTau181,将阿尔茨海默病与其他神经退行性疾病区分开来。越来越多的证据也表明,这种特异性延伸到急性脑损伤。例如,急性中风和创伤性损伤与总tau和NFL水平的增加有关,而pTau181水平保持不变。该研究结果为潜在地将手术与脆弱患者的AD的后续发展联系在一起的致病过程提供了新的见解。重要的是,考虑到这项研究的样本量小,随访时间有限,需要更大规模的纵向调查来进一步探索这一潜在的联系。
生物标志物的增加在心脏手术中被强调,这导致术后神经认知障碍的风险比非心脏手术更高。心脏手术的特定参数,包括体外循环和潜在的循环骤停和低温的需要,可能会增加神经元损伤和随后的认知功能下降的风险。血浆生物标记物可能有助于识别患者和基于手术的术后神经认知障碍的风险,并有助于制定将风险降至最低的方案。然而,超越围手术期并同时评估认知的研究需要将围手术期的生物标记物图谱与长期认知结果联系起来。
文献来源:https://jamanetwork-com.washington.80599.net/journals/jamaneurology/fullarticle/2784413
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#标志物#
36
#神经退行性变#
54
#神经退行#
42
#Neurol#
41
#非心脏#
42
#大手术#
38
#Tau#
35
#生物标志#
0
#生物标志#
39
学习了,希望能有更多知识学习
60