Nat Commun:揭示淋巴结中重要信号通路,以更好理解病理生理过程
2020-02-11 不详 生物探索
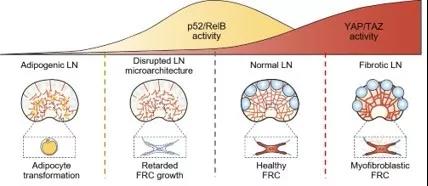
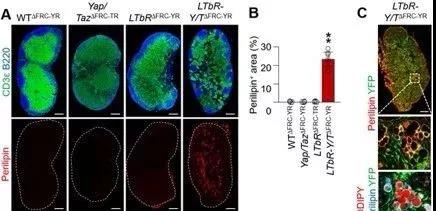
SARS、MERS以及最近的新型冠状病毒2019-nCoV等病原体已成为全球性威胁。淋巴结(LN)通过为免疫细胞的生长提供庇护所并抵抗病原体,从而与传染病作斗争。但是,人们对LN的特定内部运作方式知之甚少。韩国基础科学研究所(IBS)的科学家们发现Hippo-YAP/TAZ信号通路在LN的形成和维持中起主要作用。该研究报告发表在《Nature Communications》杂志上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#COMMUN#
31
#Nat#
32
#病理生理#
35
#淋巴结#
25
#信号通路#
34