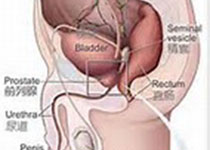
Oncogene:TXNDC9能够调控氧化应激诱导的雄激素受体信号来促进前列腺癌恶化
2019-09-15 AlexYang MedSci原创
活性氧(ROS)和ROS诱导的氧化应激与前列腺癌(PCa)发展和肿瘤去势抵抗性的恶化相关。该过程部分的是通过雄激素受体(AR)信号的激活。然而,ROS激活AR的潜在机制仍旧不清楚。最近,有研究人员报道了包含硫氧还蛋白结构域蛋白9(TXNDC9)是ROS激活AR信号的一个重要的调节因子。TXNDC9的表达可以由ROS诱导上调,TXNDC9表达的上调与晚期临床阶段有关。TXNDC9还能促进PCa细胞生
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Gene#
24
#雄激素受体#
33
#应激#
37
#Oncogene#
27
前列腺癌相关研究,学习了,谢谢梅斯
40