BMJ:高流量供氧对大多数疑似急性冠脉综合征患者没有益处
2021-03-03 MedSci原创 MedSci原创
目前的临床实践指南建议是,不应该给非低氧血症合并ST段抬高型心肌梗死(STEMI)或非STEMI的患者供氧。
50多年来,尽管只有有限的证据表明氧气可以改善急性心肌梗死患者的预后,但它已经被用于治疗急性心肌梗死。补充氧气可以纠正或减少低氧血症,这在急性冠脉综合征(ACS)患者中很常见。然而,一些证据表明,动脉血氧饱和度水平高于正常值可能会导致冠状动脉收缩或增加氧化应激。目前的临床实践指南建议是,不应该给非低氧血症合并ST段抬高型心肌梗死(STEMI)或非STEMI的患者供氧。

pixabay.com
然而,现有的证据有其局限性。首先,纳入随机试验的患者通常风险较低,可能不能代表所有接受常规治疗的患者。其次,所有先前的试验都没有足够的能力来确定氧疗在死亡率上的绝对差异。第三,在以前的试验中,大多数患者的血氧饱和度正常。吸氧的好处可能需要患者存在低氧血症。起始氧的饱和阈值和供氧时的目标氧饱和度是不确定的。第四,氧的作用可能取决于诊断,例如,急性STEMI患者通常有长期和严重的心肌缺血,可能比其他疾病患者获益更大。
为了确定高流量补充氧与疑似急性冠脉综合征(ACS)患者30天死亡率之间的关系,有研究者进行了一项实用的、随机的高氧与低氧输注策略的比较,作为常规护理的一部分,对新西兰两年来接受心脏急救护理的一大组患者进行了研究。该研究结果近日发表在BMJ杂志上。
40872名疑似或确诊的急性冠脉综合征患者在研究期间被纳入全新西兰急性冠脉综合征质量改善登记册或救护车ACS路径。20304例采用高氧方案,20568例采用低氧方案。ST段抬高型心肌梗死(STEMI)和非ST段抬高型心肌梗死的最终诊断根据登记和ICD-10出院代码确定。
在两年的时间里,四个地理区域被随机分配到两个氧气治疗方案。高氧方案建议在缺血症状或心电图改变时使用面罩供氧6-8 L/min,而不考虑血氧饱和度(SpO2)。低氧方案建议只在动脉血氧饱和度低于90%时使用氧,目标动脉血氧饱和度低于95%。主要结局为30天全因死亡率。
研究结果发现,两种氧疗方案治疗的患者的个人和临床特征非常匹配。对于疑似ACS的患者,高氧组和低氧组的30天死亡率分别为613(3.0%)和642(3.1%)(比值比0.97,95%可信区间0.86到1.08)。4159例(10%)ST段抬高型心肌梗死患者中,高氧组和低氧组的30天死亡率分别为8.8%(n=178)和10.6%(n=225)(0.81,0.66~1.00),10218例(25%)非ST段抬高型心肌梗死患者的30天死亡率分别为3.6%(n=187)和3.5%(n=176)(1.05,0.85~1.29)。
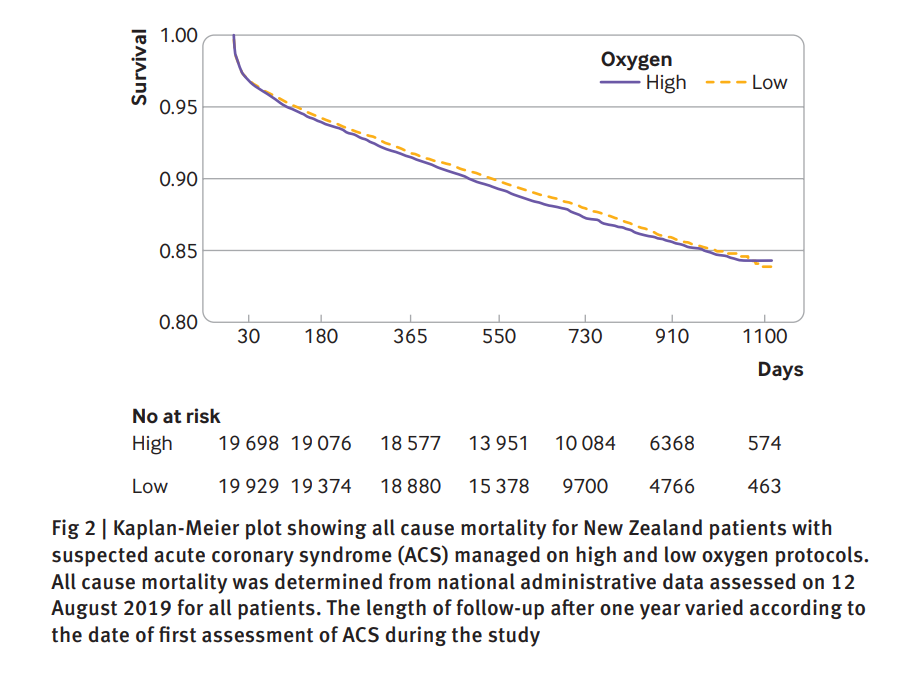
Kaplan-Meier图显示新西兰疑似急性冠状动脉综合征(ACS)患者在高氧和低氧治疗方案下的所有原因死亡率。
这项研究发现,对于怀疑患有急性冠脉综合征的广大普通患者,推荐高流量氧疗治疗缺血性症状或缺血心电图改变作为常规护理的一部分,这既无益处,也无坏处。这一发现与之前的研究一致,表明高流量氧不太可能使大多数假定为缺血性胸痛且氧饱和度正常的患者受益。由于氧被广泛使用,因此确定它是否与危害有关是很重要的。
参考文献:Ralph A H Stewart, et al. High flow oxygen and risk of mortality in patients with a suspected acute coronary syndrome: pragmatic, cluster randomised, crossover tria. BMJ 2021; 372 doi: https://doi.org/10.1136/bmj.n355 (Published 02 March 2021)Cite this as: BMJ 2021;372:n355
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













好东西学习了
71
#BMJ#
40
#综合征#
43
学习了
88
学习了!
85
感谢分享
73