Heart:血小板计数对经皮冠状动脉介入治疗患者的意义
2022-06-08 MedSci原创 MedSci原创
低血小板计数与主要出血风险相关,而高血小板计数仅与缺血事件相关。
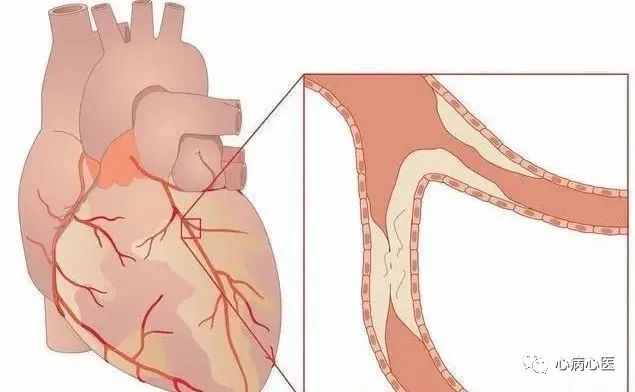
经皮冠状动脉介入治疗(PCI)是冠状动脉疾病(CAD)患者最常进行的血管重建手术。虽然PCI的长期结局已经改善,但这些患者仍然存在发生不良临床结局的风险,包括缺血和大出血并发症。血小板基线计数与PCI后患者临床结局之间的关系尚未明确。
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员进行了剂量反应和两两荟萃分析,以更好地描述初始血小板计数的预后价值和PCI术后患者的临床结局。
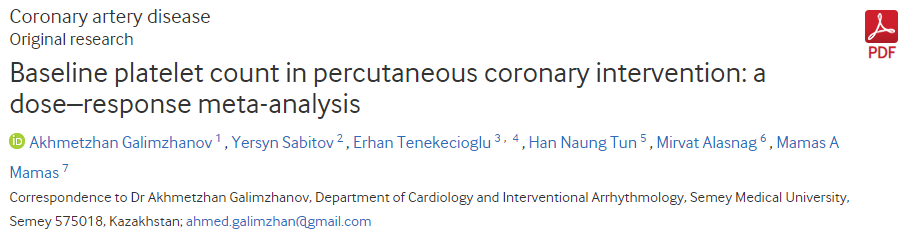
研究人员检索了PubMed、Scopus和Web of Science数据库(检索时间截止到2021年10月9日),以明确血小板计数和PCI术后临床结局之间关系的研究。该研究的主要研究结局为全因死亡率、主要不良心血管事件(MACE)和大出血。研究人员通过随机效应两两和单阶段剂量-反应荟萃分析,计算了HR和95%CI。
该分析纳入了19项研究,共计217459例患者。研究人员报告了基线血小板计数与随访时全因死亡、MACE和大出血之间呈J形关系。在低血小板计数时出血事件的风险超过血栓事件的风险(<175×109/L),而在高血小板计数时观察到主要的缺血风险(>250×109/L)。两两荟萃分析显示,初始血小板计数与出院后全因死亡率、大出血风险(对于血小板减少:风险比为1.39,95%可信区间(95%CI)为1.30-1.49;风险比为1.51,95%CI为1.15-2.00)和任何原因以及MACE导致的死亡(血小板增多症:风险比为1.60,95%CI为1.29-1.98;风险比为1.47,95%CI为1.22~1.78)之间存在密切联系。
由此可见,低血小板计数与主要出血风险相关,而高血小板计数仅与缺血事件相关。
原始出处:
Akhmetzhan Galimzhanov.et al.Baseline platelet count in percutaneous coronary intervention: a dose–response meta-analysis.heart.2022.https://heart.bmj.com/content/early/2022/05/24/heartjnl-2022-320910
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#冠状动脉介入治疗#
37
学习了
32
#经皮冠状动脉介入治疗#
36
#ART#
30
#血小板计数#
51
#HEART#
26