IBD:炎症性肠病患者处于疾病活动期是新冠肺炎病情加重的危险因素
2022-04-12 xuyihan MedSci原创
炎症性肠病是一类多种病因引起的异常免疫介导的肠道慢性及复发性炎症,有终生复发倾向,溃疡性结肠炎和克罗恩病是其主要疾病类型。
COVID-19 的发病机制是基于宿主对病毒的免疫反应的正面和负面影响之间的微妙平衡。一方面,免疫系统的激活可以减少病毒复制;另一方面,促炎细胞因子的过度产生(所谓的“细胞因子风暴”)可能有利于最严重形式的 COVID-19 的发展。由于慢性炎症、针对病毒的免疫反应以及患者使用的免疫调节药物的作用之间的相互作用,这种情况在患有慢性免疫介导疾病(包括炎症性肠病 (IBD))的患者中更为复杂。目前的证据表明,IBD 患者和普通人群在 COVID-19 的发病率和主要临床结果(即住院率、呼吸辅助需求、死亡)方面没有差异,但仍然有部分研究提出了疑议。本项研究的目的是评估 IBD 患者感染 SARS-CoV-2 的临床特征,包括 COVID-19 相关症状、干预措施和结果,并调查 COVID-19 不良结果的潜在危险因素。
这项回顾性观察性研究的纳入人群来自西西里炎症性肠病网络 (SN-IBD) 队列的连续 IBD 患者,这些患者在治疗期间被诊断为 SARS-CoV-2 感染。以及部分来自第二次 COVID-19 大流行浪潮(2020 年 9 月至 2020 年 12 月)的患者。研究人员分析了与 COVID-19 临床结果相关的人口统计学、IBD 特征和治疗以及合并症的数据,以期对相关危险因素进行进一步分析。
本项研究共纳入了 122 名患者(平均年龄 43.9 ± 16.7 岁;男性,50.0%;克罗恩病,62.3%;溃疡性结肠炎,37.7%)的临床数据。12 名患者发生 COVID-19 相关肺炎(9.8%),4 名(3.3%)需要呼吸辅助(非机械通气或经口气管插管),4 名患者死亡(病死率,3.3%)。在多变量分析中,年龄(优势比 [OR],1.034;95% CI,1.006–1.147;P= .032)和处于严重 IBD 活动期(OR,13.465;95% CI,1.104–164.182;P=.042)是 COVID-19 相关肺炎的独立预测因子,而严重的IBD疾病活动(OR,15.359;95% CI,1.320–178.677;P=.030) 是严重 COVID-19 的唯一独立预测因子,即患者需要呼吸辅助或出现死亡。据报道,肿瘤坏死因子 α 抑制剂对肺炎发展具有保护作用的趋势 ( P=.076)。
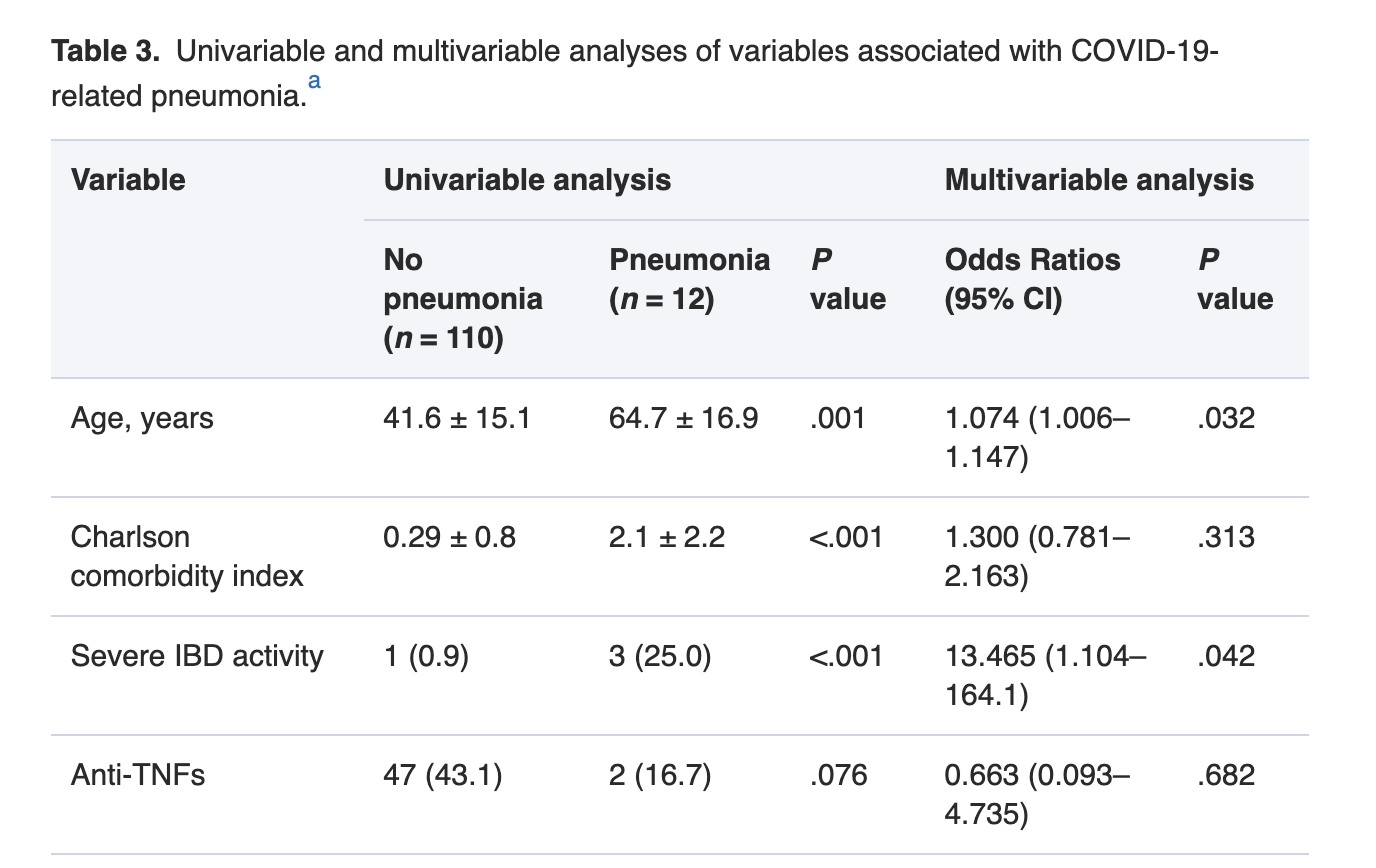
图:新冠肺炎病情加重的危险因素
这项对炎症性肠病和严重急性呼吸综合征冠状病毒 2 型感染的新冠肺炎患者的回顾性观察研究表明,严重炎症性肠病活动是新冠肺炎的疾病加重的唯一独立危险因素。
原始出处:
Fabio Salvatore Macaluso. Et al. Severe Activity of Inflammatory Bowel Disease is a Risk Factor for Severe COVID-19. Inflammatory Bowel Diseases.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#病情加重#
38
#病情#
49
#疾病活动#
43
#IBD#
34
#炎症性#
41
#炎症性肠病患者#
36