Cancer Res:SIRT3的转录抑制增强了线粒体顺乌头酸酶的激活并促使侵袭性前列腺癌到骨质的转移
2020-11-09 AlexYang MedSci原创
代谢失调是癌症进展的一个已知标志,然而促进代谢适应性以驱动转移性癌症的致癌信号仍不清楚。
代谢失调是癌症进展的一个已知标志,然而促进代谢适应性以驱动转移性癌症的致癌信号仍不清楚。

最近,有研究人员表明,雄激素受体(AR)及其核心调控因子类固醇受体共激活因子(SRC-2)对线粒体去乙酰化酶sirtuin 3(SIRT3)的转录抑制增强了线粒体顺乌头酸酶(ACO2)的活性,且有利于前列腺癌的侵袭。ACO2促进线粒体枸橼酸盐的合成以促使脂质从头生成,ACO2的基因敲除降低了总脂质含量,并能剧烈的抑制体内前列腺癌的进展。ACO2上的单一乙酰化标记赖氨酸258作为调控基序发挥作用,乙酰化缺失的Lys258Arg-突变体在酶学上无活性,不能挽救ACO2缺失细胞的生长。ACO2的乙酰化受到SIRT3的可逆调控,而SIRT3在包括前列腺癌在内的许多肿瘤中主要受到抑制。从机制上讲,SRC-2结合AR形成一个抑制复合物,可招募组蛋白去乙酰化酶2(HDAC2)到SIRT3启动子上,SRC-2的缺失可增强SIRT3的表达,同时减少了ACO2的乙酰化。在人类前列腺肿瘤中,ACO2活性显著升高;SRC-2表达增加以及伴随的SIRT3减少是前列腺癌转移病灶中的遗传标志。
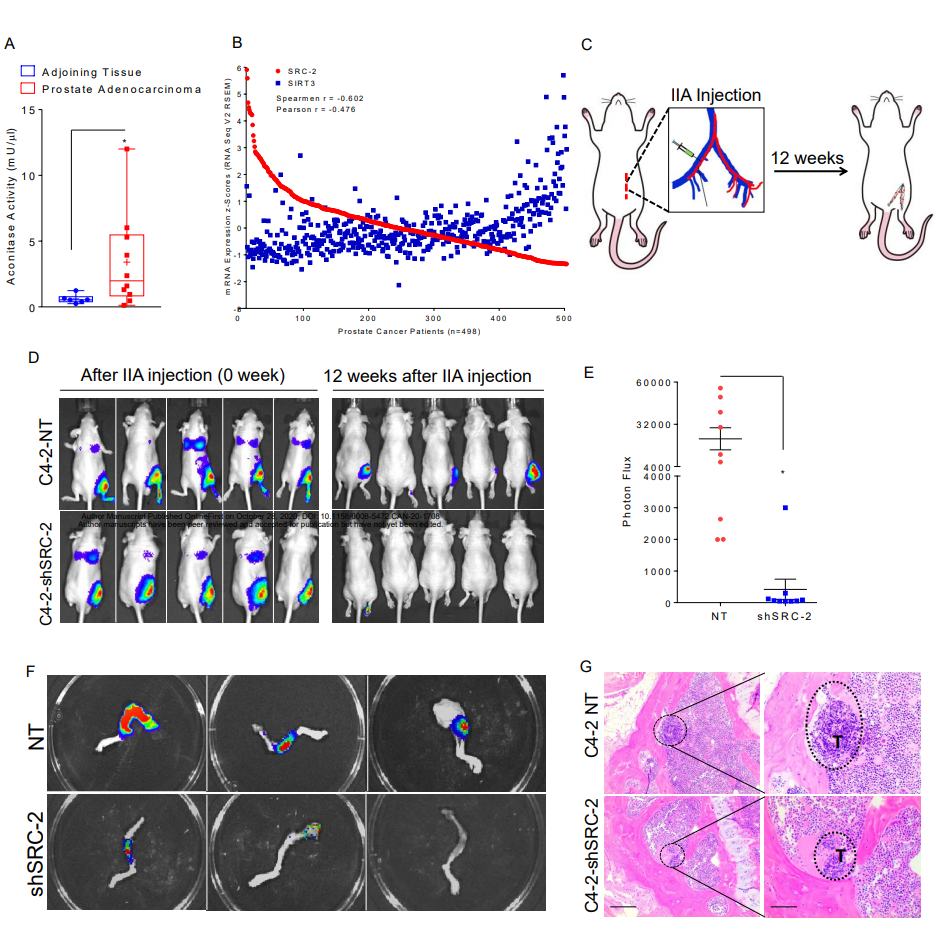
SRC-2抑制SIRT3促使侵袭性转移前列腺癌转移到骨组织
最后,研究人员在自发骨转移的小鼠模型中发现,抑制SRC-2能够重新激活SIRT3的表达,并足以清除前列腺癌在骨微环境中的定植,表明该核-线粒体调节轴是转移能力的决定性因素。
原始出处:
Abhisha Sawant Dessai, Mayrel Palestino Dominguez , Uan-I Chen et al. Transcriptional repression of SIRT3 potentiates mitochondrial aconitase activation to drive aggressive prostate cancer to the bone. Cancer Res. Oct 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#SIRT3#
32
学习了
75
#侵袭性#
45
#骨质#
36
#转录#
33
前列腺癌相关研究,学习了,谢谢梅斯
51