Liver Cancer:影像学应答是伴有肉眼血管侵犯(MVI)的晚期肝细胞癌患者应用TACE+RT治疗时的显著预后指标
2021-12-08 yd2015 MedSci原创
研究表明,影像学应答是伴有MVI的晚期肝细胞癌患者应用TACE+RT治疗时的显著预后指标。
2021年12月7日,Liver Cancer杂志上在线发表了一项来自韩国学者的研究结果,主要是评估经动脉化疗栓塞(TACE)联合放疗(RT)治疗未经治疗的伴有肉眼血管侵犯(MVI)肝局限型细胞癌(HCC)患者的影像学应答率,并分析其在总生存期(OS)结果中的临床重要性。
研究回顾性筛选2010年1月至2015年12月间接受TACE+RT作为一线治疗原发性肝癌合并MVI的患者。根据修改的实体瘤疗效评价标准(mRECIST),在完成RT后2和4个月进行影像学疗效评估。在2和4个月进行进行单变量和多变量分析。
研究期间1332例HCC合并MVI患者接受TACE + RT联合治疗,共评估467例患者。2个月时20例患者未进行影像学评估被排除,纳入427例患者。4个月时72例患者未进行影像学评估被排除,纳入355例患者。患者整体中位年龄为57岁(范围34-87),89.0%为男性。肝肿瘤最大直径中位数为9.6 cm(范围1.1-21.1),276例(64.6%)患者肝功能为Child-Pugh A级,多数患者为多发性(70.7%)和浸润型(83.8%)。超过一半的患者(56.4%)被诊断为主/双侧门静脉和/或下腔静脉侵犯。
根据治疗应答情况进行分组时,出现应答组肝功能良好的患者比例显著高于对照组(P <0.001),良好评分状态(P = 0.008),单发肿瘤(P = 0.002),结节性肿瘤(P = 0.002),肿瘤较小(P <0.001),单侧血管受累(P<;0.001),肿瘤标志物水平降低(α -胎蛋白,P = 0.042;维生素K缺乏或拮抗剂- ii [PIVKA-II]诱导的蛋白;P<0.001)。
所有患者的中位随访时间为13.1个月(范围为2.3-126.8)。到最后一次随访时,39例(9.1%)患者存活;1年、2年和5年OS发生率分别为53.9%、26.5%和11.7%,中位OS持续时间为13.1个月(95% CI, 11.6-14.9)。PFS的中位持续时间为7.4个月(95% CI, 6.6-8.4)。
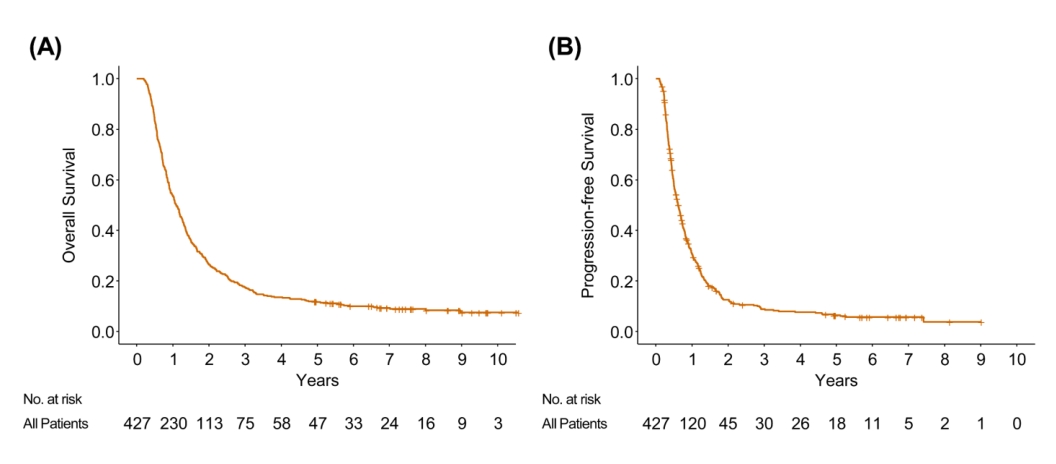
OS和PFS
在完成RT后2个月,210例(49.2%)患者观察到影像学应答(CR, 39例[9.1%];PR, 171[40.1%])。4个月时,355例可评估患者中有184例(51.8%)患者出现影像学应答(CR, 67例[18.9%];PR,117[32.9%])。
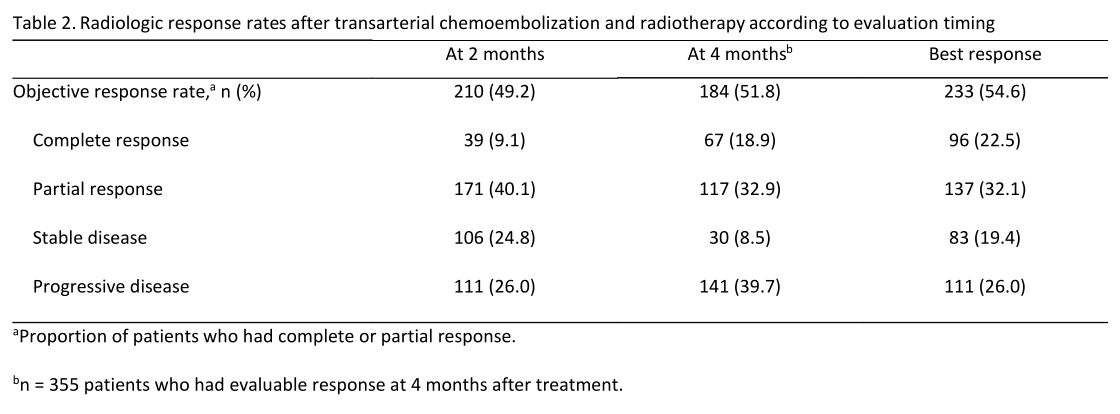
疗效评估
2个月时应答患者的中位OS为23.1个月 (95% CI, 20.1–26.6),较无应答患者显著延长(8个月,95% CI: 6.9–8.7)。4个月时应答者的中位OS为26.5个月(95% CI, 22.8 31.5),较无应答患者显著延长(9.3个月;95% CI, 8.6 10.2)。
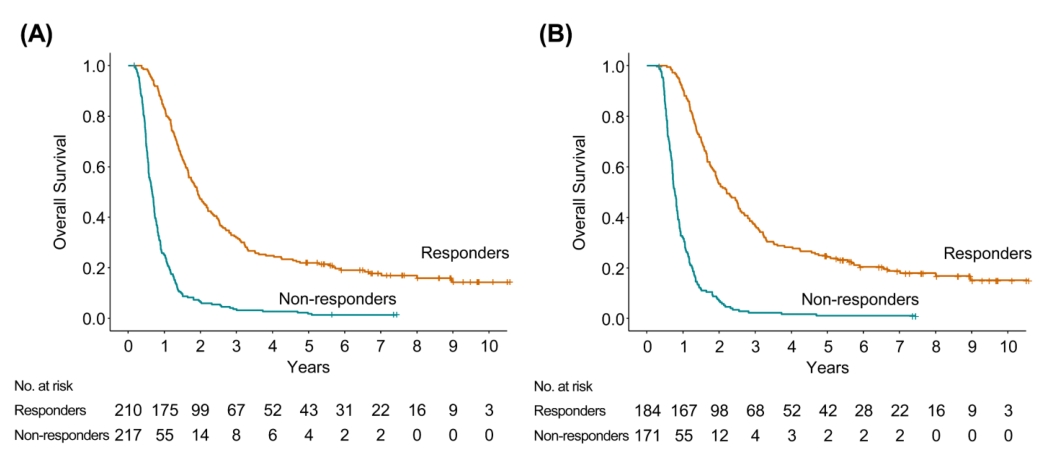
2个月和4个月时应答和无应答患者的OS对比
多变量时间依赖的Cox回归分析显示,2个月时影像学应答(HR, 3.194;95% CI 2.455 4.156, P<0.001)、Child-Pugh分级(P = 0.031)、多样性(P = 0.014)、肿瘤大小(P = 0.046)和肝内进展(P = 0.026) 是OS的独立预后因素。同样在4个月时评估分析,4个月时影像学应答(HR, 4.534;95% CI, 3.391 6.062, P<0.001), ECOG评分状态(P = 0.020)、Child-Pugh分级(P = 0.012)、多样性(P = 0.005)和肝内进展(P = 0.038) 仍然是OS的独立预后因素。
综上,研究表明,影像学应答是伴有MVI的晚期肝细胞癌患者应用TACE+RT治疗时的显著预后指标。
原始出处:
Jung J, Joo JH, Kim SY, et al. Radiologic response as a prognostic factor in advanced hepatocellular carcinoma with macroscopic vascular invasion after transarterial chemoembolization and radiotherapy. Liver Cancer , DOI: 10.1159/000521227. Published online: December 7, 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#TAC#
52
#细胞癌#
47
#ACE#
45
#肝细胞#
51
#晚期肝细胞癌#
43
#预后指标#
52