European Radiology:使用全心脏覆盖CT扫描仪评估心房颤动患者TAVI术后的图像质量和诊断性能
2022-01-12 shaosai MedSci原创
经导管主动脉瓣植入术(TAVI)术前的CT成像是评估入路、主动脉尺寸、主动脉结构和钙化的主要影像学手段。
 经导管主动脉瓣植入术(TAVI)术前的CT成像是评估入路、主动脉尺寸、主动脉结构和钙化的主要影像学手段。此外,由于动脉疾病对手术结果和预后的不利影响,也建议术前应用CT进行动脉疾病的筛查。有创冠状动脉导管造影(ICA)被作为TAVI候选人术前排除梗阻性冠状动脉疾病(CAD)的金标准。
经导管主动脉瓣植入术(TAVI)术前的CT成像是评估入路、主动脉尺寸、主动脉结构和钙化的主要影像学手段。此外,由于动脉疾病对手术结果和预后的不利影响,也建议术前应用CT进行动脉疾病的筛查。有创冠状动脉导管造影(ICA)被作为TAVI候选人术前排除梗阻性冠状动脉疾病(CAD)的金标准。
由于高心率(HR)和心率变化导致的运动和阶梯状错位伪影会显著影响图像质量和诊断效果,因此在有房颤(AF)的TAVI候选人中进行CCTA扫描极具挑战。最近,一种结合了0.28旋转时间和16厘米Z轴覆盖率的CT扫描仪引入临床,可实现在一次心跳中对患者进行全心扫描,在处理由高心率和心率不齐引起的运动伪影方面功能强大。据我们所知,还没有一项研究关注单次心跳、前瞻性心电图触发的CCTA采集在有房颤的TAVI候选人身上的应用。
近日,发表在European Radiology杂志的一项研究评估了在 TAVI 计划 CT 期间使用全心脏覆盖 CT 扫描仪评估 TAVI 房颤患者的 CCTA 图像质量和诊断性能,以进行阻塞性 CAD 筛查,为房颤患者提供了一个更可耐受、更准确的检查手段。
本研究回顾性地分析了88名连续的房颤TAVI候选人(50名男性,74±6岁),每位患者均同时接受了TAVI规划的CT和有创冠状动脉导管成像(ICA)。以ICA结果为参考标准,计算了TAVI规划CT在每个血管和每个患者层面上检测病变的准确性。同时,对图像质量、造影剂量和有效剂量(ED)进行了评估。采用5级视觉量表(1-5)来评估主观的图像质量。测量了左主冠状动脉(LM)、左前降支(LAD)、左回旋状动脉(LCX)和右冠状动脉(RCA)的CT值和信噪比。
CCTA的ED为3.25 ± 1.39 mSv,造影剂量为58.14 ± 12.34 mL。共分析了1371(1371/1408=97.4%)个直径大于1.5毫米的节段。在主观评价方面,整体图像质量的平均得分是3.99±0.96。LM、RCA、LCX和LAD的平均CT值都在400HU以上。对于检测>50%的狭窄,TAVI规划CT在每个血管和每个病人的基础上分别提供97.06%和100%的敏感性,96.23%和89.06%的特异性,99.7%和100%的阴性预测值,以及73.3%和77.4%的阳性预测值。
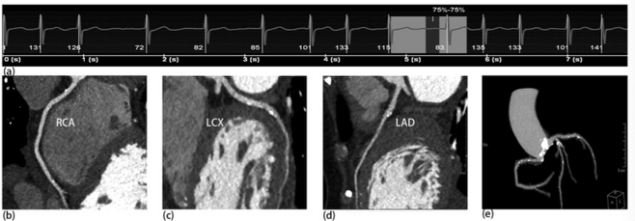
图 80岁的有房颤的主动脉瓣移植患者中进行了TAVI规划CT,心电图显示扫描时心率为135bpm。a心电图显示扫描时的心率为135 bpm。CCTA的整个冠状动脉树的图像显示在b-e。
使用宽探测器、全心覆盖扫描仪的TAVI规划CT显示出良好的冠状动脉CT血管造影图像质量,在排除有心房颤动的TAVI候选人的阻塞性冠状动脉疾病方面具有较高的敏感性和阴性预测价值。
原文出处:
Yu Zhang,Zhenlin Li,Yongchun You,et al.Image quality and diagnostic performance evaluation in transcatheter aortic valve implantation candidates with atrial fibrillation using a whole-heart coverage CT scanner.DOI:10.1007/s00330-021-08187-z
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PE#
32
#诊断性#
0
#CT扫描#
27
#心房#
30
不错不错
50
#学习#学习
52
学习了
39
学习#学习#
44