干货:颅脑损伤患者的紧急救治
2022-02-23 “院前急救联盟 ”公众号 “院前急救联盟 ”公众号
颅脑外伤又称创伤性颅脑损伤(TBI),因脑组织的特殊生理功能,其损伤后的致残率和死亡率在各种类型的创伤中位居首位。
颅脑外伤概述
颅脑外伤又称创伤性颅脑损伤(TBI),因脑组织的特殊生理功能,其损伤后的致残率和死亡率在各种类型的创伤中位居首位。是一种常见的创伤,是指在外界暴力的作用下,使头部和脑部受伤的统称,在全身各部位损伤中,其发生率仅次于四肢损伤。伤情复杂严重,致残率和死亡率较高。
多见于交通、 工矿、高空作业等事故, 自然灾害、 爆炸、 火器伤、 坠落、 跌倒以及各种锐器、 钝器对头部的伤害。经抢救治疗,大部分患者虽然幸存下来,但常遗留有不同程度的神经功能障碍。诸如意识、运动、感觉、言语、认知功能、排便排尿等方面的障碍。
常见病因
(1) 直接损伤 是指暴力直接作用于颅脑造成的损伤, 根据力的作用方向不同, 分为加速性损伤,减速性损伤和挤压性损伤。
A:加速性损伤:暴力打击后头部由静止转为运动,损伤效应为:①打击部位的冲击点伤;②暴力作用对侧的对冲性损伤。前者损伤重。
B:减速性损伤:运动的头部突然撞在外物上,头部由运动转为静止,损伤效应主要为对冲性脑损伤,其次为局部的冲击点伤。
C:挤压伤:头部两侧相对的外力挤压而致伤,多见于产伤。
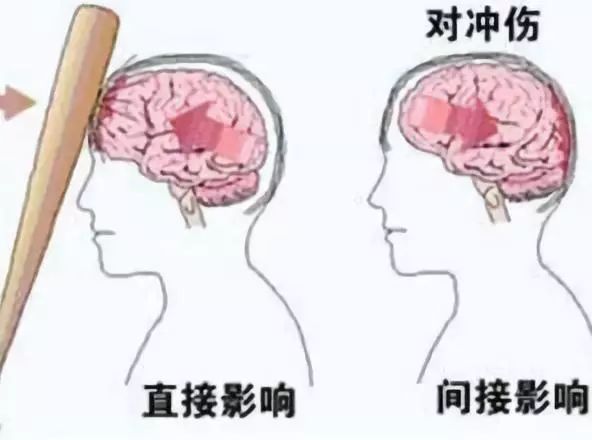
(2) 间接损伤 是指暴力作用不在头部, 而在远离头部的身体其他部位而后传递到颅脑造成的颅脑损伤,是特殊而严重的损伤类型。包括头颅与脊柱连接处损伤、 挥鞭性损伤、 创伤性窒息和暴震伤等。
A:挥鞭样损伤:头部受力后沿力作用的方向往复运动,引起颅颈交界处的剪应力伤。惯性作用尚可使脑内不同结构的界面上发生剪应力性损伤。
B:颅颈连接处损伤:臀或双足着地的坠落伤时,暴力沿脊柱传达至枕骨髁部,致枕骨大孔环形陷入骨折,后组脑神经和延髓和(或)上颈髓损伤。
C:胸部挤压伤:即创伤性窒息。胸部突受压力冲击,上腔静脉血逆行注入颅内,致使颅内出血。
病理生理
1. 中枢系统:①在原发性脑创伤的局灶性区域,脑血流(CBF)和脑氧代谢率(CMRO2)降低。随着颅内压(ICP)升高,颅内更多的组织出现低灌注和低代谢;②当ICP持续升高时,CBF自主调节能力被削弱;同时合并的低血压将进一步加重脑组织缺血;③血脑屏障破坏导致的血管源性脑水肿和缺血导致的细胞毒性脑水肿将进一步增高ICP,从而加重脑组织缺血和缺氧,甚至引起致命性的脑疝。
2. 循环系统:由于继发性交感神经兴奋和/或颅内高压引起的库欣反射,存在低血容量的闭合性颅脑创伤患者常表现为高血压和心动过缓。镇静镇痛药物的使用、甘露醇和速尿的降颅压措施、打开硬脑膜的手术操作和/或合并其他器官损伤致大量失血时,都可使TBI患者出现严重的低血压、心动过速、心律失常和心排血量下降。心电图常见T波、U波、ST段、QT间期等异常表现。
3. 呼吸系统:颅脑创伤患者可出现低氧血症和异常的呼吸模式(如自主过度通气),并经常伴有恶心呕吐和反流误吸。交感神经兴奋可引起肺动脉高压,导致神经源性肺水肿。
4. 体温:发热可进一步加重脑损伤。
临床分类
(1)临床应用分类
1)开放性损伤(头皮挫伤、裂伤、撕脱伤、开放性颅骨骨折)。
2)闭合性损伤(头皮下血肿、帽状腱膜下血肿、骨膜下血肿、颅骨线状骨折、凹陷骨折、无内开放的颅底骨折)。
3)开放性颅骨与脑损伤(火器性颅脑穿透伤或非穿透伤)。
4)开放性颅底骨折。
5)闭合性原发性脑损伤(脑震荡、脑挫裂伤、弥散性轴索损伤、原发性脑受压即单纯凹陷性骨折或乒乓凹陷)。
6)闭合性原发性脑损害(单发硬膜下、硬膜外、脑内、脑室内血肿、颅内多发血肿、迟发性血肿、脑水肿肿胀)。
(2)按照是否原发进行分类
1)原发性颅脑外伤:指机械撞击和加速减速挤压作用于颅骨和脑组织立即造成的局灶性或弥散性损伤,主要有脑震荡、弥漫性轴索损伤、脑挫裂伤、原发性脑干损伤及下丘脑损伤。
2)继发性颅脑外伤:通常在原发性颅脑创伤后数分钟、数小时或数天后发生的神经组织的进一步损伤。继发性损伤包括:①全身情况:低氧血症、高碳酸血症或低血压;②形成硬膜外、硬膜下、脑内血肿或血肿增大;③持续的颅内高压症状。脑缺血和缺氧是导致和加重继发性脑损伤的主要原因。
(3)伤情轻重分类:按昏迷时间、阳性体征及生命体征表现分为轻、中、重、特重4型。
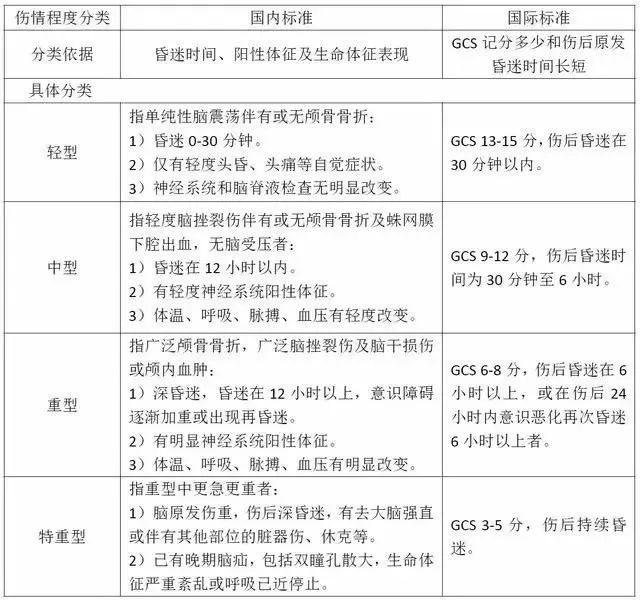
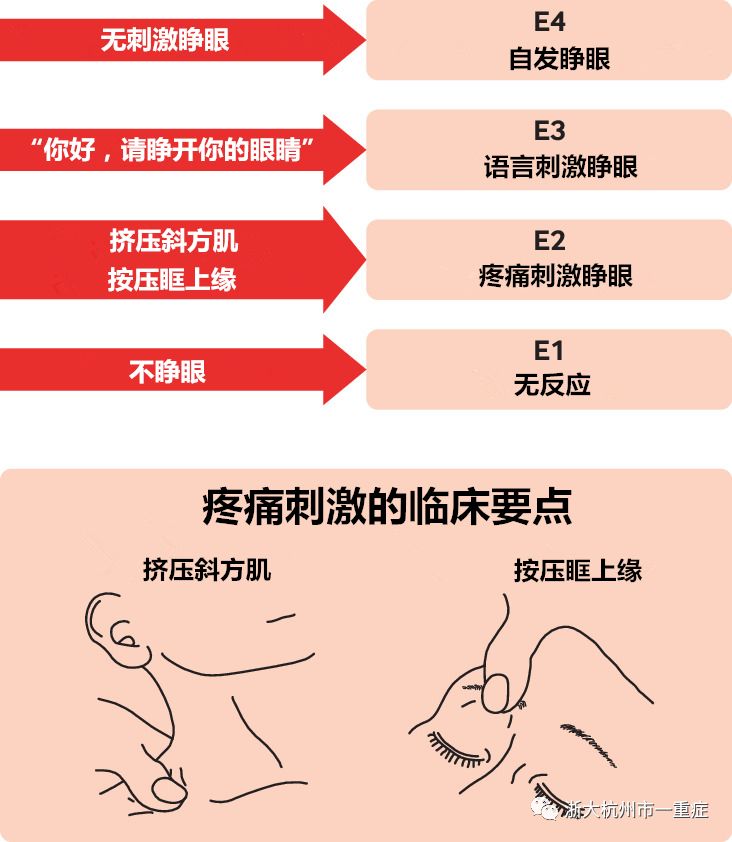
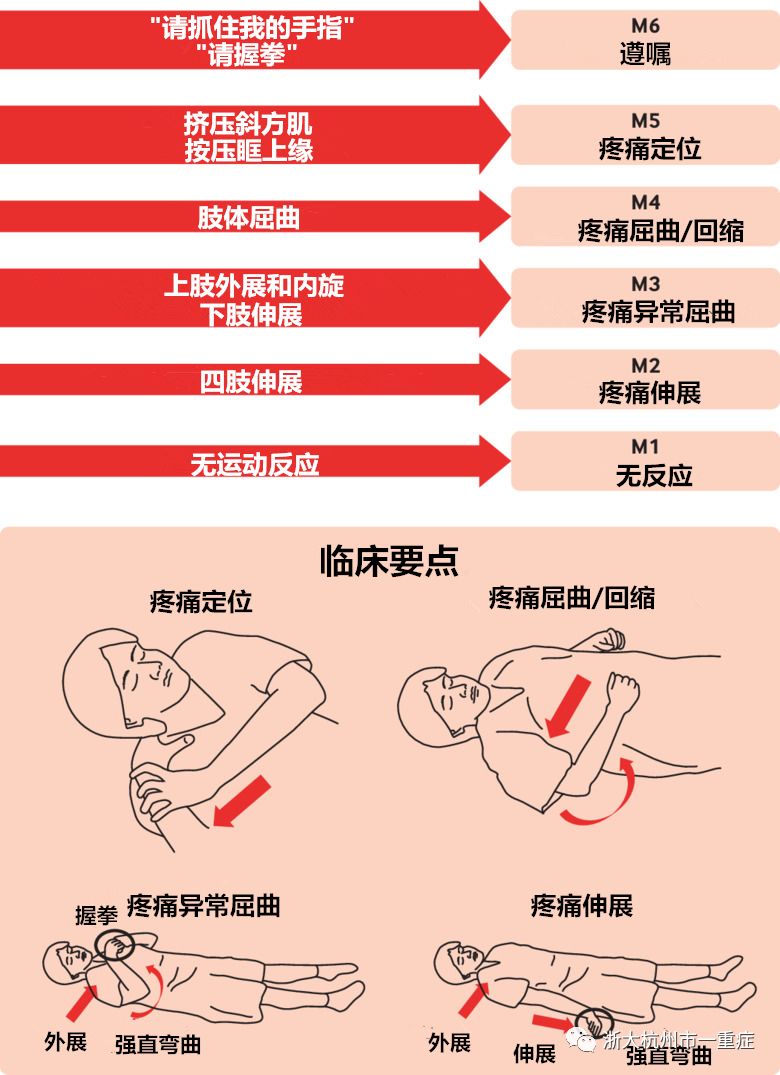
(4)昏迷程度分类:GCS(Glasgow coma scale)昏迷分级。
格拉斯哥评分(GCS)是医学上评估病人昏迷程度的方法,在临床上主要用于评估脑外伤病人的病情及预后,是由英国格拉斯哥大学的两位神经外科教授GrahamTeasdale与BryanJ.Jennett在1974年发明的测评昏迷的方法?

睁眼反应
运动反应
语言反应
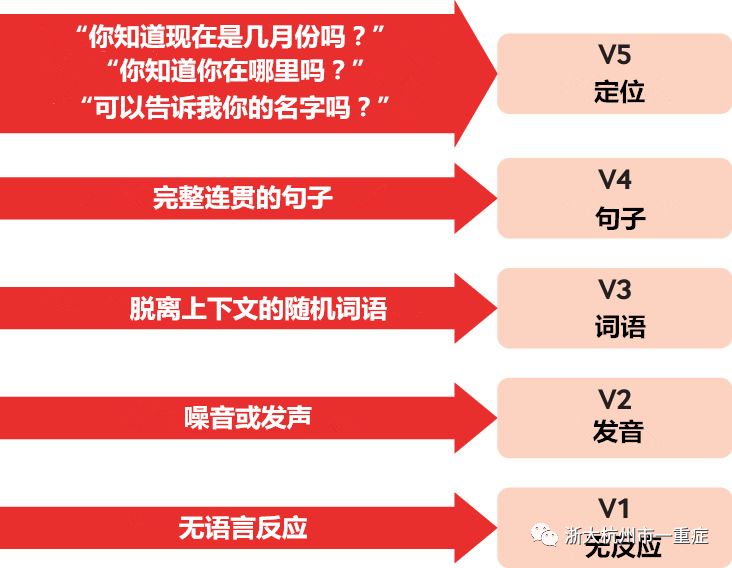
GCS包括睁眼反应、运动反应和语言反应3个部分,总分最高15分,最低3分。临床上常用GCS量表对颅脑患者进行分型,其中13~15分为轻型,9~12分为中型,3—8分为重型,GCS<4分表示预后不良。GCS量表因其量化指标少,具有简单便于记忆的突出优点。
(5)颅脑损伤按照严重程度:包括脑震荡, 脑挫裂伤, 颅内血肿、脑水肿、脑疝等。
A:脑震荡:通常是指头部受到外力打击后,即刻出现短暂的脑功能障碍,并可导致短暂昏迷、近事遗忘、以及头痛、恶心、呕吐、认知和情感障碍等一系列症状,但神经系统检查无阳性发现。
1. 短暂的意识丧失,一般不超过半小时。
2.近事遗忘,即对受伤前后的经过不能回忆。
3.神经症状如头痛、恶心呕吐、眩晕、畏光、乏力等。
4.植物神经紊乱如心慌、血压下降、面色苍白、冷汗等。
5.精神症状如烦躁、悲伤、抑郁、紧张、焦虑、兴奋等。
B:脑挫裂伤是脑挫伤和脑裂伤的统称,脑挫伤指软脑膜尚完整者;脑裂伤指软脑膜、血管和脑组织同时有破裂,伴有外伤性蛛网膜下腔出血。(两者常同时并存,临床上又不易区别,故常合称为脑挫裂伤)
(1)意识障碍:伤后立即出现,意识障碍的程度与时间与损伤程度、范围直接相关。一般以>30分钟为限。
(2)局灶性症状与体征:依损伤部位和程度而定,有偏瘫、失语等。
(3)头痛、恶心、呕吐:与颅内高压、蛛网膜下腔出血有关或植物神经功能紊乱,要注意排除血肿。
(4)生命体征:轻中度挫伤生命体征变化不明显;重度挫伤出现继发性脑水肿或颅内血肿→ICP↑ → BP↑、P↓、R ↓、瞳孔不等大及锥体束征,应高度怀疑脑疝可能。
(5)脑膜刺激:蛛网膜下腔出血所致,头痛、畏光,脑膜刺激征(+)。
C:颅内血肿分为硬膜外血肿、硬膜下血肿、颅内血肿和脑室内血肿。
1、硬脑膜外血肿;意识障碍:昏迷-清醒-再昏迷;颅内压ICP升高;动眼N损伤引起患侧瞳孔散大;锥体束征:病变对侧伤后一段时间出现或呈进行性加重的肢体活动障碍。
CT检查,可发现在硬膜与颅骨之间有一双凸镜或弓形高密度阴影,可有脑室受压,中线移位情况。
2、硬脑膜下血肿;意识障碍:进行性加重;ICP增高;瞳孔改变;神经系统体征;CT:脑表面出现半月性、新月性的高密度影。
3、脑内血肿:主要由脑挫裂伤导致的脑实质内血肿,临床表现同硬膜下血肿。
D:脑水肿:
脑损害症状 :多发生在局部脑挫裂伤灶的周围。常见的症状为癫痫与瘫痪症状加重,或因水肿范围扩大,波及语言运动中枢引起运动性失语。脑损伤后,如症状逐渐恶化,应多考虑脑水肿所致。弥漫性脑水肿,可因局限性脑水肿未能控制,继续扩展为全脑性,或一开始即为弥漫性脑水肿。
颅内压增高症状:表现为头痛、呕吐加重,躁动不安,嗜睡甚至昏迷。眼底检查可见视乳头水肿。早期出现生命体征变化,脉搏与呼吸减慢,血压升高的代偿症状,如脑水肿与颅内压高继续恶化则可导致发脑水肿生脑疝。
其他症状:脑水肿影响额叶、颞叶、丘脑前部可以引起精神障碍,严重者神志不清、昏迷。颅内压增高也可引起精神症状。有时体温中度增高,脑水肿累及丘脑下部,可引起丘脑下部损害症状。
E:脑疝
脑疝为最严重的表现, 小脑幕切迹疝最常见, 表现为对侧肢体偏瘫和进行性意识恶化, 最终导致脑干功能性衰竭。
小脑扁桃体疝则因后颅窝占位性病变或幕上占位性病变导致全颅内压增高所致, 出现血压升高, 双侧锥体束征, 急性者常突发呼吸障碍、 昏迷, 甚至迅速死亡。
临床表现
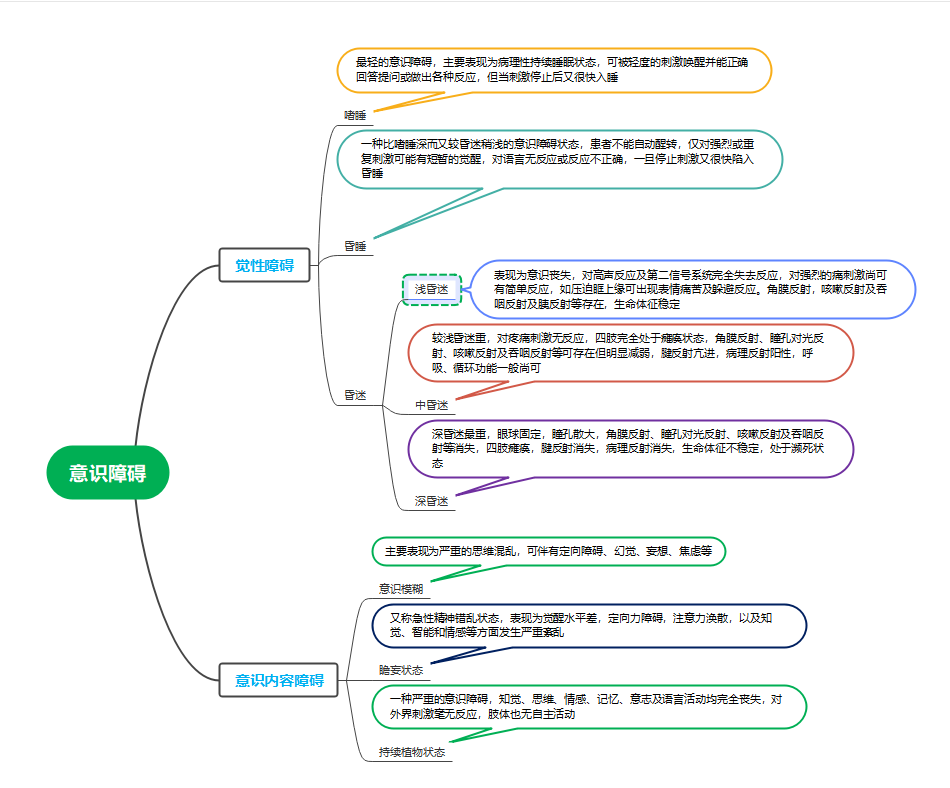
1、意识障碍:
2、头痛、呕吐
受伤局部可有疼痛。但头部多呈持续胀痛,常伴有恶心和喷射状呕吐。
3、生命体征改变
体温、呼吸、脉搏、血压可以反应颅脑损伤的程度。生命体征正常或轻微变化多表示伤情较轻,病情平稳;生命体征变化较大多提示病情危重,急需处理,如血压升高、脉压差加大,心率缓慢或异常加快,呼吸深慢和节律不规整等。
4、眼部征象
由于颅脑损伤病人多有昏迷,观察瞳孔、眼球运动及眼底改变可较客观地了解病情。
瞳孔:正常人直径为3-4mm,小儿略大,双侧等大等圆;脑疝时,早期:患侧瞳孔缩小,光反射迟钝。晚期:瞳孔散大,光反射消失。一侧瞳孔大,伴意识障碍,多是小脑幕切迹疝。
正常眼球位置对称,各方向运动灵活,如有同向凝视或固定,或视轴散开等提示颅内受损。
眼底检查如发现视乳头水肿、出血等提示颅内高压或眼球内受伤。
5、神经系统局灶症状与体征
颅脑受伤后可以出现一种或多种症状:随意运动、言语、精神活动的异常;失语、书写不能;记忆力、计算能力差;躯体麻木、肢体单瘫或偏瘫、肌张力失调;尿崩、高热、消化道出血;全身强直;共济运动失调;吞咽不能、声音嘶哑,口角歪斜等。
急救与治疗
及时、正确地处理急性颅脑损伤能明显改善患者预后,所谓“及时” 、“正确”应当包括:现场急救首先要处理伤后发生的误吸、舌后坠和呼吸暂停等,及由此而导致的缺氧、二氧化碳蓄积。
1. 急救原则及急救处理
急救原则:先救命后治病;先稳定生命体征后病因治疗;选用最快捷有效的诊断治疗方法
保持呼吸道通畅,解除呼吸道梗阻,清楚口鼻腔异物,必要时建立人工气道,人工或机械辅助呼吸。
头部及其他部位伤口应立即进行止血包扎。
如果血压较低需要建立输液通道,防治休克。
必要的全身检查,以便确定是否存在多发伤,确定优先处理的顺序。
伤口再污染的防止和感染的早期预防,预防破伤风的发生。
2. 手术指征
颅内有占位病变,如硬膜外、下或脑内血肿的患者,伴有以下指征单侧瞳孔扩大者,务必及时手术: ① 有局部脑受压症状;② 中线移位>5 mm;③ ICP>25 mmHg;④ 有脑疝的征象者。开放性伤口,如头皮裂开、颅骨凹陷、硬膜缺损和脑组织外露等。后颅凹血肿。广泛性脑挫裂伤,意识出现进行性恶化, 颅高压危象者,可考虑行大骨瓣减压术。危重患者如有双瞳孔散大、去大脑强直及呼吸停止者,手术多无益。弥漫性轴索损伤、弥漫性脑肿胀,应在密切观察下采用非手术治疗,当出现症状恶化时可采取与广泛脑挫裂伤相似处理方式。
3. 非手术治疗
颅脑外伤的非手术治疗主要包括两个部分, 即全身状态的维持和降低颅内压
(1)全身状态的维持:抬高头部 10~20o,避免颈部过度屈曲及包扎过紧。有助于静脉血液回流。昏迷患者因丧失吞咽动作而易导致口腔细菌孳生,故应保持口腔清洁,有助于降低肺部并发症。尽早放置胃管,行胃肠减压、 减轻腹胀;通过引流的胃液, 尽早发现胃粘膜出血病变;给予胃肠道进食, 以保护胃肠粘膜屏障功能。预防应激性溃疡。纠正低氧血症及高碳酸血症, 昏迷患者均应建立人工气道, 估计昏迷超过 3~5 天者可考虑行气管切开。纠正低血压和低脑灌注压(CCP) , CPP=平均动脉压(MAP) -颅内压(ICP) 。如果 ICP 高至 25 mmHg, 欲维持 60 mmHg 的灌注压, MAP 则至少要求达至 80 mmHg 以上, 否则容易导致脑缺血。
(2) 脱水治疗:脑水肿是构成颅内压增高的主要因素之一, 所以控制脑水肿的发生和发展是降低颅内压关键之一。20%甘露醇静脉滴注, 注药后半小时降到最低水平, 每次 0.5~1 g/kg, 可重复使用。利尿药因有利尿脱水作用, 导致血液浓缩, 渗透压增高, 从而使脑组织脱水与颅内压降低, 常用呋塞米, 每次0.5~2.0 mg/kg, 注射后 5~10 min 开始利尿, 1~2 小时发挥最大作用, 可与甘露醇交替使用。10%甘油溶液静脉注射, 成人每日 500 ml, 共使用 5~6 天。
(3) 糖皮质激素的应用:糖皮质激素具有抑制氧自由基导致的脂质过氧化反应;稳定膜的离子通道;抑制磷脂酶 A2, 减少花生四烯酸的释放, 有利于脑脊液重吸收, 而不是直接作用;最终产生抗水肿作用。
首选地塞米松, 一次 10 mg, 以后每 6 小时一次, 一周后逐渐停药。其次可选用氢化可的松, 5%葡萄糖或生理盐水稀释后静脉滴注, 100~800 mg/天。大剂量激素应用可能导致胃肠道出血, 糖代谢障碍, 免疫系统抑制, 皮肤损伤及创口愈合延迟。
(4) 脑功能保护:应用脑代谢功能活化剂, 如吡硫醇、 甲氯芬酯和胞磷胆碱等, 具有复活及增强脑代谢, 适度地刺激脑神经功能, 改善脑血流作用。应用神经生长因子, 具有促神经突起生长和神经元细胞数目增多作用。神经节苷脂具有保持膜结构功能, 对钙离子具有高度亲和力, 减少钙离子内流;调节营养因子, 促进神经再生, 减少病灶周围细胞死亡和调节神经递质功能。
(5) 冬眠亚低温疗法:将体温控制在 32~34℃, 对严重脑挫裂伤, 脑干或丘脑损伤伴高热和去大脑强直患者, 有较好治疗作用。冬眠亚低温疗法除可使脑血流量下降, 脑体积缩小, 颅内压降低外, 还可以降低脑代谢率, 增加脑缺氧的耐受性, 改善细胞通透性防止脑水肿发生发展。常用的冬眠合剂有冬眠Ⅰ号(氯丙嗪 50 mg, 异丙嗪 50 mg, 哌替啶 100 mg) , 冬眠Ⅱ号(异丙嗪 50 mg, 哌替啶 100 mg, 海得琴0.6 mg) , 冬眠Ⅲ号(异丙嗪 50 mg, 哌替啶 100 mg) , 冬眠Ⅳ号(异丙嗪 50 mg, 哌替啶 100 mg, 乙酰丙嗪 20 mg) 。
(6) 高压氧治疗:高压氧治疗是指在高压氧舱内 1 个大气压以上的纯氧, 通过人体血液循环以携带更多的氧到病损组织和器官, 增加血氧弥散和组织内的氧含量, 迅速改善和纠正组织缺氧, 防止或减轻缺氧性损害的发生和发展, 促进病损组织的修复和功能恢复, 从而达到治疗或抢救的目的。
颅脑外伤患者在生命体征稳定的前提下, 排除颅内活动性出血, 早期高压氧治疗是一个重要原则。最佳治疗时间为伤后 3 天内。重型颅脑外伤高压氧治疗压力为 0.2~0.25 MPa, 60 分钟, 1 次/日, 10~12 次为 1 个疗程。高压氧通过改善病灶区脑组织缺氧, 减轻脑水肿、 降低颅内压力, 纠正缺氧, 促进代谢而恢复神经电位活动;促进侧支循环的形成, 保持损伤病灶周围的缺血半影区的神经细胞产生脑保护作用。
护理措施
1.非手术治疗护理措施
(1)严密观察
生命体征,意识、瞳孔及时发现病情变化。
(2)注意病情变化:
颅脑损伤的病情特点是多变、易变、突变、难以预测,即使已经手术多天的患者仍可在手术后出现突然变化,因此有效、及时的病情动态观察有着重要的意义。一般颅脑损伤病情观察为72小时,以后根据病情和医嘱继续观察。
(3)颅内压增高的动态观察:
颅脑损伤引起的血肿、脑挫裂伤或脑组织肿胀引起颅腔容积与颅内容物体积之间的平衡失调,超过生理调节功能的限度时出现颅内压增高,当颅内压>1.76kPa(180mmH2O)时,患者可出现剧烈头痛、喷射性呕吐、血压升高(收缩压升高),在观察过程中如发现这些先兆症状时要警惕脑疝的发生,及时与医生联系采取措施。
(4)意识观察:
意识改变是颅脑损伤患者最常见的体征之一。它往往能反映大脑皮质和脑干网状结构的功能状态。根据意识动态观察可判断伤情的转归。意识障碍的类型在临床上可分为清醒、嗜睡、浅昏迷、中昏迷、深昏迷。可以通过对话、呼唤姓名、定时及定向力测定来判断,对昏迷患者通过疼痛刺激(如针刺、压眶上神经、压胸骨柄等)后观察其有无呻吟、皱眉、肢体运动及各种反射(吐咽反射、咳嗽反射、睫毛反射等)的出现。清醒后患者又出现嗜睡→浅昏迷→深昏迷提示颅内有血肿形成,需立即手术治疗。脑干损伤患者处于昏迷状态,逐渐出现咳嗽、吞咽等生理反射,肢体出现运动,病理征消失,这些征象说明病情在好转。相反,原来清醒的转为嗜睡,对周围反应迟钝,躁动的转为安静、昏睡,并出现病理征,则提示病情在恶化。
(5)癫痫发作的患者
应注意观察发作前的征兆,发作时注意保持呼吸道通畅,保护患者的安全,及时遵医嘱使用抗癫痫药物,并给予患者吸氧,纠正癫痫发作所致的脑缺氧情况,发作后准确记录癫痫发作及持续的时间以及发作类型等。
(6)注意观察有无上消化道出血等并发症的发生。
(7)早期发现继发性颅内出血和颅内压增高,及时进行手术治疗。
(8)早期发现继发脑神经损害,及时处理。
(9)保护患者安全
①对于癫痫和躁动不安的患者,应给予专人护理。
②在癫痫发作时应注意保护患者。
③烦躁患者床旁加床栏,适当约束防止患者受伤。
(10)解除呼吸道梗阻,防止误吸。
①患者置于侧卧位,床旁备吸引器,随时吸出患者呕吐物,口鼻腔分泌物、血块等。
②立即给患者吸痰。
③必要时置口咽通气道或行气管插管。
④注意观察患者的血氧饱和度。
(11)高热患者给予物理降温或遵医嘱给予降温药物治疗。
(12)药物治疗的护理
①应用脱水药物的护理:
在神经外科脱水治疗中,20%甘露醇为常用的脱水药物,其次为甘油果糖等。由于脱水药物的药理作用及神经外科疾病特点,护士在使用20%甘露醇等脱水药物时需注意如下几点。
a.保证输液速度:
20%甘露醇能够提高血浆渗透压,形成血管及脑组织之间的渗透压差,导致脑、脑脊液水分进入血管内,从而降低颅内压和脑脊液容量及其压力。lg甘露醇可产生渗透浓度为5.5mOsm/L,注射100g甘露醇可使2000ml细胞内水转移至细胞外,尿钠排泄50g。甘露醇注射后10~20分钟颅内压开始下降,半小时将至最低水平,1小时开始回升,4~8小时回升到用药前的水平。临床中甘露醇的输注速度以10~15ml/min为宜。为保证甘露醇的滴速。在输液时选择型号合适的静脉留置针,向患者及家属讲明快速输注的目的,避免家属调整滴速。
b.静脉血管的选择:
由于甘露醇滴速较快,易刺激局部产生疼痛,严重者发生静脉炎,使静脉变硬。因而在静脉穿刺时,宜选择较相直的静脉,由于静脉管径及血流因素,可减轻药液对血管壁的刺激,减少静脉炎的发生。
e.注意病情观察:
由于20%甘露醇为渗透性脱水剂,使组织间隙的水分向血管内转移,可引起一过性血压升高,诱发继续出血。另外,甘露醇使血肿以外的组织脱水后,使血肿.脑组织间的压力梯度增大,从而促使血肿扩张或加重活动性出血。在护理过程中,护士密切巡视患者,注意患者的意识、精神状态、血压、脉搏的变化。另外,注意患者是否出现神志淡漠、烦躁不安、尿量减少等症状,警惕水电解质紊乱、肾功能损害等药物不良反应,及时通知医生进行检查及处理。
②应用激素药物的护理:
由于有些糖皮质激素,具有很强的抑制脂质过氧化作用,维持细胞膜与细胞器膜的稳定性,维持细胞内外钙、钠、钾、氯等离子稳态平衡,维持脑组织血流量及改善Na+-K+-ATP酶的功能,保护神经细胞的有氧代谢,使脑水肿得到改善等功能。针对神经外科患者进行激素治疗时,护士需要严格遵照医嘱给药,给药期间注意有无因应用激素诱发应激性溃疡、感染等不良反应。
(13)心理护理:
对清醒患者作适当的解释,让患者知道某些症状可随时间的延长而逐渐消失,以清除患者的恐惧心理,对于昏迷患者,应主动安慰家属,稳定家属的情绪。
(14)健康宣教
①轻型患者应鼓励其尽早自理生活和恢复活动,注意劳逸结合:瘫痪患者制定具体计划,指导协助肢体功能的锻炼。
②原发性颅脑损伤有的可留下不同程度的后遗症,某些症状可随时间的延长而逐渐消失。对有自觉症状的患者,应与患者及家属及时沟通,给予适当的解释和宽慰,鼓励患者保持乐观情绪,主动参与社交活动。
③有癫痫发作者不能单独外出,应按医嘱长期定时服用抗癫痫药物。
④如原有症状加重时应及时就诊。
⑤3~6个月后门诊影像学复查。
2.手术治疗护理措施
(1)术前护理措施
①心理护理:解释手术的必要性、手术方式、注意事项:鼓励患者表达自身感受:教会患者自我放松的方法:针对个体情况进行针对性心理护理:鼓励患者家属和朋友给予患者关心和支持。
②饮食护理:急行手术者应该立即禁食禁饮:择期手术者术前8小时禁食禁饮:饱胃患者应行胃肠减压,防止麻醉后食物反流引起窒息。
③术前检查:
协助完善相关术前检查:血常规、尿常规、肝肾功能检查、心肺功能、磁共振、CT等。
术前准备:
a.交叉配血,以备术中用血;
b.进行抗生素皮试,以备术中、术后用药;
c.剃头、备皮、剪指甲、更换清洁病员服;
d.遵医嘱带入术中用药;
e.测生命体征,如有异常或患者发生其他情况,及时与医生进行联系;
f.遵医嘱给予术前用药;
g.准备好病历、CT片、MRI片等以便带入手术室。
④与手术室人员进行患者、药物核对后,送入手术室。
(2)术后护理措施
①全麻术后护理常规:
了解麻醉和手术方式,术中情况、切口和引流情况;持续吸氧2~3L/min,持续或间断吸氧,能够改善脑缺氧,使脑血管收缩,降低脑血流量;持续心电监测生命体征。
②伤口观察及护理:
观察伤口有无渗血渗液,若有异常应及时通知医生并更换敷料:观察头部体征,有无头痛、呕吐等。
③饮食护理:
术后6小时内禁食禁饮,6小时后遵医嘱更改饮食。
④各管路观察及护理:
输液管保持通畅,留置针妥善固定,注意观察穿刺部位皮肤,尿管按照尿管护理常规进行,一般清醒患者术后第2日可拔出尿管,拔后注意关注患者自行排尿情况。
⑤疼痛护理:
评估患者疼痛情况.注意头痛的部位、性质,结合生命体征等综合判断。
⑥基础护理:
做好口腔护理、尿管护理、定时翻身、雾化、患者清洁等工作。
⑦癫痫的观察和护理。
⑧高颅内压的观察及护理。
⑨药物治疗护理:同术前药物治疗护理。
3.并发症的处理及护理
(1)上消化道出血
①临床表现:患者胃管内抽出咖啡色胃内容物,患者出现柏油样便、腹胀、肠鸣音亢进,重者可有呕血或大量便血,面色苍白,脉搏快速,血压下降等休克征象。
②处理:严密观察生命体征;遵医嘱应用止血药和抑制胃酸分泌的药物:经胃管用冰盐水反复抽吸后注入云南白药等药物止血;必要时行胃肠减压,并做好大量失血的各项抢救准备工作。
(2)癫痫的护理:癫痫发作的患者应注意观察发作前的征兆,发作时注意保持呼吸道通畅,保护患者的安全,及时遵医嘱使用抗癫痫药物,并给予患者吸氧,纠正癫痫发作所致的脑缺氧情况,发作后准确记录癫痫发作及持续的时间以及发作类型等。
(3)颅内压增高的护理
①遵医嘱按时测量生命体征,严密观察患者神志、瞳孔及生命体征的变化。
②患者出现意识障碍加深,呼吸、脉搏减慢,而血压升高等颅内压增高典型表现,经常提示有颅内血肿或急性水肿,应立即通知医生采取处理。
(4)肺部感染
①临床表现:患者常有发热、痰多,血象增高,肺部出现干、湿啰音,胸部x线有助于诊断。
②处理:鼓励患者咳嗽排痰,协助患者定时翻身、叩背:不能有效地清除呼吸道分泌物的患者,应给予负压抽吸,必要时可行气管插管或气管切开,有利于保持呼吸道通畅:痰液黏稠者可行雾化吸入:加强口腔护理,以免口咽部细菌误吸入下呼吸道造成感染。
(5)下肢深静脉血栓
①临床表现:下肢水肿、浅静脉怒张、患肢胀痛。
②处理:严密观察肢体皮肤温度、色泽、弹性及肢端动脉搏动情况;抬高患肢,给患者穿弹力袜或间断使用抗血栓压力泵以促进静脉血回流;一旦发生深静脉血栓,下肢应抬高制动,局部湿热敷,禁止按摩。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














学习学习
45
#颅脑损伤#
43
#损伤#
47
#紧急#
51
学习了,谢谢分享
48
早期小肿瘤非小细胞肺癌(NSCLC)伴有肺胸膜
51
学习了,很全面
50
内容很丰富
45
学习
29
学习新知识
26