BMC Med:肥胖、代谢风险与坚持健康生活方式:英国生物库的前瞻性队列研究
2022-03-01 从医路漫漫 MedSci原创
有争议的证据表明,肥胖对有健康生活方式的人的健康没有风险,特别是如果没有肥胖的代谢并发症。

背景:有争议的证据表明,肥胖对有健康生活方式的人的健康没有风险,特别是如果没有肥胖的代谢并发症。该研究的目的是在不同的身体质量指数(BMI)类别中,研究坚持生活方式建议与不发生或致命心血管疾病的代谢并发症和全因死亡率之间的关系。
方法:这项当代前瞻性队列研究包括339,902名基线无心血管疾病的成年人,从英国生物库(UK Biobank)于2006年至2010年招募,随访至2018-2020年。主要暴露于四种健康的生活方式行为:从不吸烟,酒精摄入量≤112克/周,150分钟中等体育活动或75分钟剧烈活动/周,每天≥5份水果或蔬菜,我们评估了这些整体和整个BMI组。过度肥胖的代谢并发症包括高血压、糖尿病和高脂血症,我们研究了在没有这些并发症的情况下,肥胖是否与风险增加有关。结果包括全因死亡率、死于心血管疾病和心血管疾病(CVD)。
结果:符合四种生活方式建议但超重的人有更高的全因死亡率;对于BMI 30 ~ 34.9 kg/m2,危险比(HR)为1.42(95%可信区间为1.20 ~ 1.68);对于BMI≥35 kg/m2,危险比(HR)为2.17(95%可信区间为1.71 ~ 2.76)。这一风险较低,但对于没有代谢并发症的人来说仍然增加;在全因死亡率方面,BMI 30-34.9 kg/m2的HR为1.09 (95% CI 0.99 - 1.21), BMI≥35 kg/m2的HR为1.44 (95% CI 1.19 - 1.74)。在偶发性和致命性心血管疾病中也发现了类似的模式。
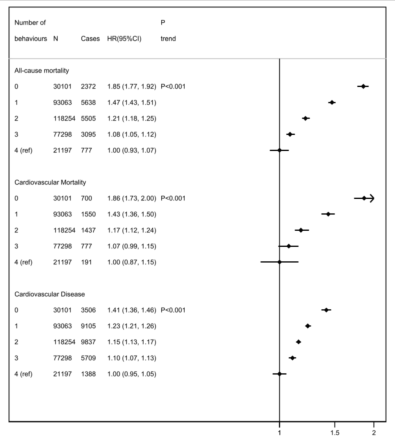
图1坚持0、1、2、3或4种健康生活方式行为的全因死亡率、心血管死亡率或心血管疾病发病率风险的Cox比例风险模型人力资源风险比;CI,置信区间(浮动)。根据年龄、性别、种族、汤森剥夺评分、教育程度、地区、心血管家族史、糖尿病家族史、绝经状态和BMI组调整多变量危险比
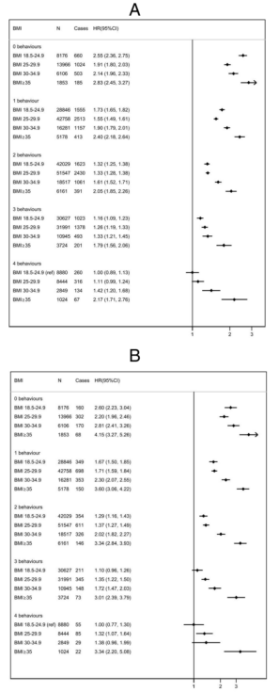
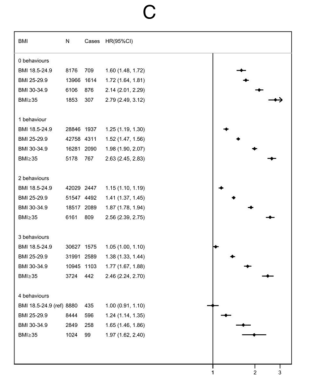
图2 BMI组(kg/m2)的全因死亡率(A)、心血管死亡率(B)和心血管疾病发生率(C)风险的Cox比例风险模型,按遵守0、1、2、3或4种健康生活方式行为进行分层。人力资源风险比;CI,置信区间(浮动);BMI:身体质量指数(kg/m2)。根据年龄、性别、种族、汤森剥夺评分、教育程度、地区、家族心血管病史、家族糖尿病史和绝经状态调整多变量风险比
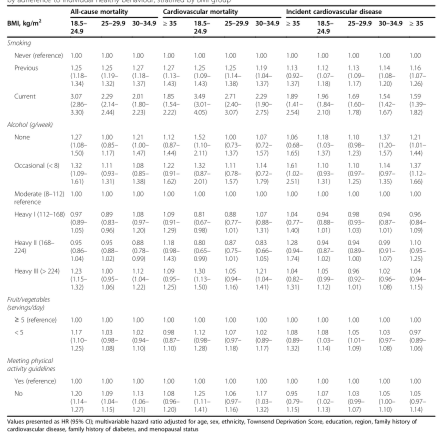
表1按BMI组分层,按个体健康行为的遵守情况建立全因死亡率、心血管死亡率或心血管疾病诊断风险的Cox比例风险模型
结论:在超重或肥胖人群中,满足健康的生活方式建议,或没有肥胖的代谢并发症,可以部分(但不是全部)抵消随后心血管疾病的风险,以及过早死亡。为实现和保持健康体重和采取健康行为提供支持可能是有效预防性保健的重要组成部分。
原文出处:Heath L, Jebb SA, Aveyard P,et al.Obesity, metabolic risk and adherence to healthy lifestyle behaviours: prospective cohort study in the UK Biobank.BMC Med 2022 Feb 15;20(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#前瞻性#
35
#前瞻性队列#
44
#前瞻性队列研究#
43
#健康生活#
43
#BMC#
25
#健康生活方式#
36
#Med#
22