Cancer Gene Therapy:CHD1缺失对R0切除的前列腺癌患者的无转移生存产生负面影响并促进体内自发转移
2021-01-24 AlexYang MedSci原创
前列腺癌(PCa)患者的治疗结果变化很大,取决于是否发生远处转移。多条染色体缺失与根治性前列腺切除术(RP)后的早期肿瘤标志物PSA复发(生化复发,BCR)有关,但其对远处转移形成的潜在作用在很大程度
前列腺癌(PCa)患者的治疗结果变化很大,取决于是否发生远处转移。多条染色体缺失与根治性前列腺切除术(RP)后的早期肿瘤标志物PSA复发(生化复发,BCR)有关,但其对远处转移形成的潜在作用在很大程度上是未知的。
最近,有研究人员具体分析了肿瘤抑制因子CHD1(5q21)的缺失是否影响手术后远处转移的风险,以及CHD1的缺失是否直接导致体内转移的形成。研究参与者>6800名,结果发现,CHD1缺失对R0患者的无转移生存率有负面影响(HR:2.32;95%CI:1.61,3.33;P<0.001),与术前PSA、pT期、pN状态、Gleason评分和BCR无关。更多的是,CHD1缺失可预测pT2患者无BCR生存期缩短,以及所有患者的癌症特异性生存期。在体内,CHD1缺失增加了两种不同PCa模型中自发性肺转移的形成,且与单细胞转移相比,多细胞克隆数量更高。转录组分析显示,在两个测试的PCa模型中,CHD1缺失后PCa特异性转移抑制因子和TGFβ信号调节因子PMEPA1下调。
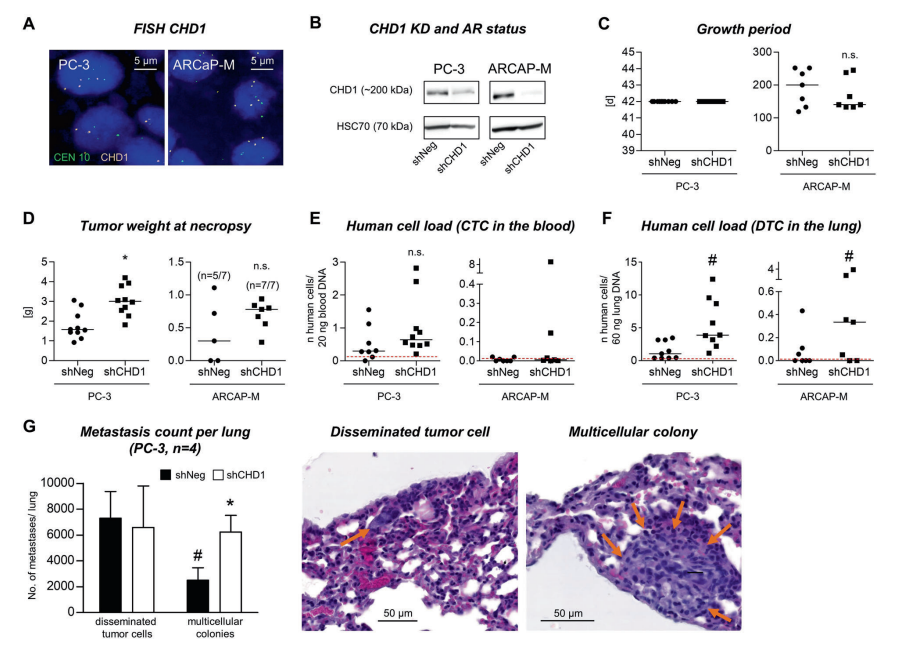
CHD1缺失对体内自发转移形成的功能作用
最后,研究人员指出,CHD1的缺失能够增加R0切除PCa患者的术后转移的风险,并促进体内自发转移的形成。
原始出处:
Su Jung Oh-Hohenhorst, Derya Tilki, Ann-Kristin Ahlers et al. CHD1 loss negatively influences metastasis-free survival in R0-resected prostate cancer patients and promotes spontaneous metastasis in vivo. Cancer Gene Therapy. Jan 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Gene#
45
#ERA#
37
#负面影响#
40
#CHD#
41
已读,受益匪浅
91
前列腺癌相关研究,学习了,谢谢梅斯
51