Front Oncol:腹腔镜与开放式根治性子宫切除术治疗2018版FIGO IA2-IIA2期宫颈癌患者的生存结果比较:倾向性评分加权分析
2021-11-20 yd2015 MedSci原创
该回顾性研究表明ORH治疗IA2-IIA2期宫颈癌患者的疗效符合NCCN指南推荐,但是某些无不良预后因素患者使用LRH治疗非劣效于ORH。
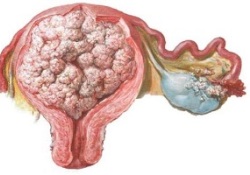
近期,Frontiers in Oncology杂志上发表了中国医科大学附属盛京医院研究团队的一项研究成果,基于2018年国际妇产科学联合会(FIGO)分期,比较开放(ORH)和腹腔镜根治性子宫切除术(LRH)治疗IA2-IIA2期宫颈癌的生存和复发结果。
研究回顾性分析2013年1月1日-2016年12月31日在中国医科大学附属盛京医院行开腹或腹腔镜子宫根治术的1373例早期宫颈癌患者的资料。基于倾向评分的处理加权逆概率(PS-IPTW)被用来平衡两组间的协变量。
2013年1月1日至2016年1月1日,共筛查1373例早期宫颈癌患者。最终纳入2009版FIGO 分期IA2-IIA2期宫颈癌患者705例,其中ORH组558例,LRH组147例。根据2018版FIGO 分期标准再分期,仍有561例患者属于IA2-IIA2期,其中ORH组437例,LRH组124例。144例患者升级至FIGO 2018期IIIC1p-IIIC2p,其中ORH组121例,LRH组23例。
ORH组中位随访时间为61个月(范围23-94个月),而LRH组中位随访时间为57.5个月(范围26-88个月)。截至2020年12月31日,入组患者中,ORH组死亡66例,复发78例,LRH组死亡22例,复发27例。ORH组5年OS率为88.4%,LRH组为83.7% (Log-Rank P=0.202)。ORH组5年PFS发生率为86%,LRH组为81.2% (Log-Rank P=0.143)。经IPTW调整后,ORH组的OS (HR= 2.095, 95%CI: 1.233-3.562, P= 0.006, Adjust Log-Rank P= 0.001)和PFS (HR=1.950, 95%CI: 1.194-3.184, P=0.008, Adjust Log-Rank P= 0.002)率明显高于LRH组。
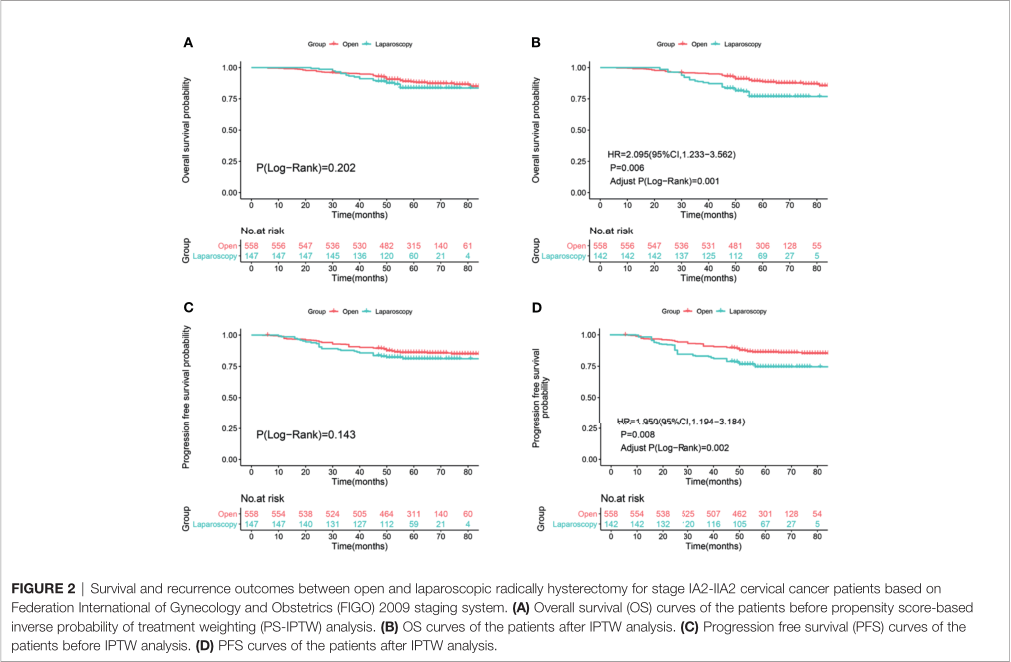
2009版FIGO分期两种治疗方式预后分析
根据2018版FIGO 分期标准再分期后, IPTW调整前两种治疗方式的OS (Log-Rank P = 0.143)和PFS (Log-Rank P = 0.137)无明显差异。ORH组和LRH组5年PFS率分别为88.6%和83.3%。然而,经过PS- IPTW分析,ORH组的OS (HR=1.977, 95%CI: 1.077-3.626, P=0.028, Adjust Log-Rank P= 0.019)和PFS (HR=1.811, 95%CI: 1.046-3.134, P=0.034, Adjust Log-Rank P= 0.023)明显优于LRH组。
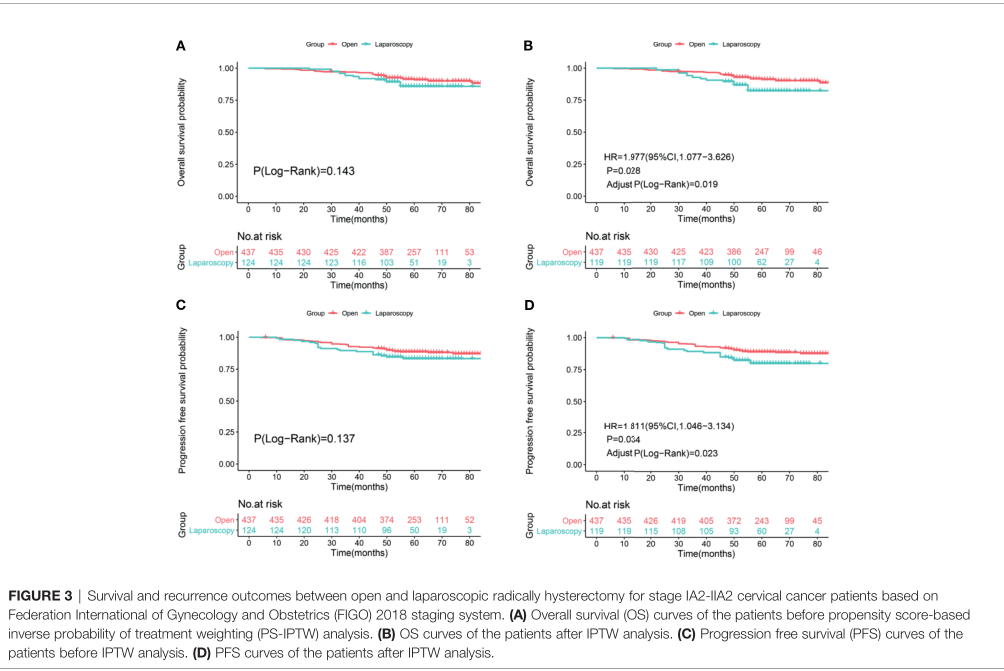
2018版FIGO分期两种治疗方式预后分析
2018版FIGO标准IIIC1p-IIIC2p期患者中,ORH组死亡26例,LRH组死亡6例,5年OS率分别为78.6%和72.2% (Log-Rank P=0.579)。ORH组27例复发,LRH组7例复发,5年PFS率分别为77%和69.6% (Log-Rank P = 0.387)。通过PS-IPTW,两组间OS (HR=1.869, 95%CI: 0.720-4.851, P=0.199, Adjust Log-Rank P= 0.212)和PFS (HR=1.004, 95%CI: 0.761-4.755, P=0.169, Adjust Log-Rank P= 0.191)率无明显差异。
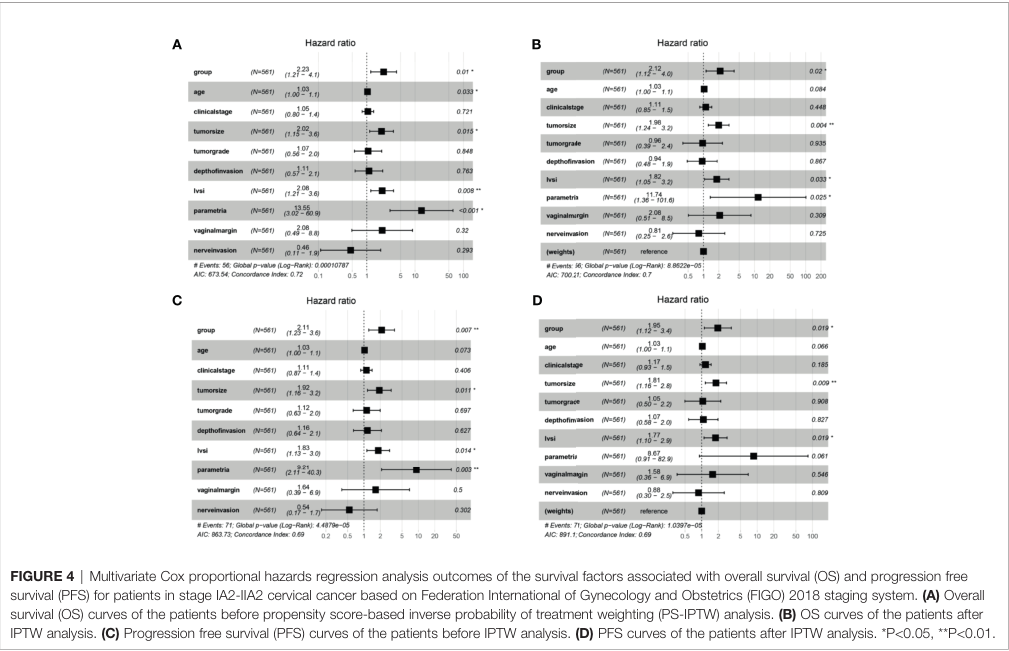
调整前,分组、年龄、肿瘤大小、LVSI和宫旁浸润被证实与宫颈癌患者的生存状况有关。同时确定分组、肿瘤大小、LVSI和宫旁浸润与患者的复发有关。IPTW调整后,肿瘤大小、LVSI均被证实与FIGO IA2-IIA2期宫颈癌患者的PFS和OS具有显著相关性。
综上,该回顾性研究表明ORH治疗IA2-IIA2期宫颈癌患者的疗效符合NCCN指南推荐,但是某些无不良预后因素患者使用LRH治疗非劣效于ORH。
原始出处:
Zhao W, Xiao Y, Zhao W, Yang Q and Bi F (2021) Survival Outcomes in Patients With 2018 FIGO Stage IA2–IIA2 Cervical Cancer Treated With Laparoscopic Versus Open Radical Hysterectomy: A Propensity Score-Weighting Analysis. Front. Oncol. 11:682849. doi: 10.3389/fonc.2021.682849
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#切除术#
33
#Oncol#
35
学习了
0
#子宫切除#
38
#学习#学习
61
#腹腔镜#
42
#子宫切除术#
37
#宫颈#
39
#根治#
47
症和危重症病人达到78,740例;全球新
61