European Radiology:从影像学角度评估胰腺癌新辅助治疗后的肿瘤可切除性和治疗反应
2022-03-07 shaosai MedSci原创
据称,新辅助治疗可以提高胰腺癌切缘阴性的概率,以提高治疗预后。
 胰腺癌是全世界范围内癌症死亡的第七大原因,估计每年有466003人死于胰腺癌。胰腺癌患者的预后较差,所有阶段的总体5年生存率在10%左右。据称,新辅助治疗可以提高切缘阴性的概率,以提高治疗预后。
胰腺癌是全世界范围内癌症死亡的第七大原因,估计每年有466003人死于胰腺癌。胰腺癌患者的预后较差,所有阶段的总体5年生存率在10%左右。据称,新辅助治疗可以提高切缘阴性的概率,以提高治疗预后。
随之而来的一个重要问题是,究竟哪些患者应该在新辅助治疗后接受手术治疗呢?现阶段,影像学检查仍是评估手术可行性的首选检查手段。然而,利用影像手段选择手术人选的障碍之一是,临床上缺乏对新辅助治疗后评估可切除性或肿瘤反应的共识。
近日,发表在European Radiology杂志的一项研究评估了六位腹部阴性科医生对胰腺癌肿瘤可切除性的评估的观察者间一致性,并衡量了影像科医生在预测阴性切缘方面的诊断性能。
本项回顾性研究纳入了2017年至2020年期间接受新辅助治疗的可切除性胰腺癌患者。由六位阅读者初始分期和再分期CT图像进行了独立评估。他们根据NCCN指南对再分期CT的可切除性进行分类,并根据我们提出的标准以5级尺度评价肿瘤对新辅助治疗的反应。采用Gwet's协议系数评估了观察者之间的一致性。使用交叉随机效应模型来汇集六位阅读者预测阴性切缘的敏感性和特异性。
共纳入了77名患者,中位年龄为66岁(59-70)。肿瘤可切除性的观察者间一致性为0.64(95%CI,0.56-0.71),区分可切除与不可切除肿瘤的一致性为0.84(0.77-0.91)。肿瘤反应等级的一致性为0.89(0.85-0.92)。当仅将再分期CT上的 "可切除 "视为指标测试阳性时,预测阴性切缘的集合敏感性和特异性分别为48%(43-52%)和61%(57-64%)。当 "可切除"'或 "边缘可切除 "被认为是阳性时,集合的敏感性和特异性分别为91%(89-94%)和5%(4-6%)。
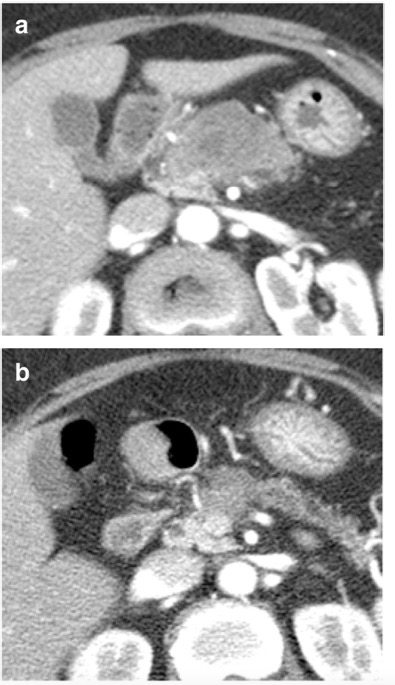
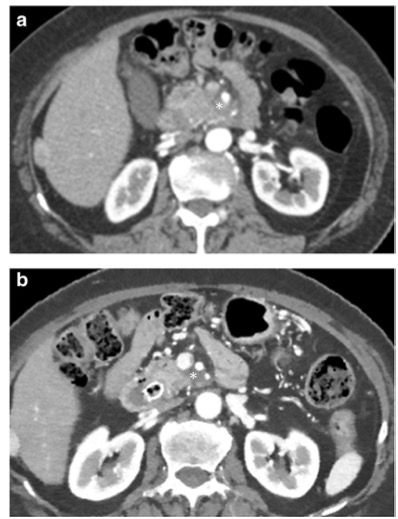
图 70岁女性,因胰腺癌接受新辅助治疗。(a)在诊断时和(b)新辅助治疗后的增强CT图像。所有六位阅读者对再分期CT的肿瘤可切除性评估为 "边缘-可切除"。五位阅读者评估肿瘤反应等级为1(反应良好)。由于肿瘤周围的纤维化和粘连,进行了门静脉/肠系膜上静脉切除和端对端吻合术,但病理检查没有静脉侵犯的证据。切缘为阴性,YpT2N0分期。
本研究表明,在区分可切除与不可切除的胰腺癌方面,以及在确定接受新辅助治疗患者再分期CT的肿瘤反应等级方面,六位放射科医生的观察者间一致性很高。CT可以可靠地进行切缘可切除胰腺癌患者的新辅助治疗后手术人选的筛选,并具有较高的观察者间一致性和敏感性。
原文出处:
Hae Young Kim,Yoon Jin Lee,Won Chang,et al.Tumor resectability and response on CT following neoadjuvant therapy for pancreatic cancer: inter-observer agreement study.DOI:10.1007/s00330-021-08494-5.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
33
#新辅助#
41
已学习
63
好知识
53
已学习
60
学习
58