IBD: 围手术期使用地塞米松可减少炎性肠病患者术后术后的炎症反应和肠梗阻的发生
2021-04-10 MedSci原创 MedSci原创
尽管生物制剂已经被广泛用于治疗炎症性肠病(IBD),但手术仍然是最终的解决方案。75%的患者在其一生中都会经历一次手术治疗。
尽管生物制剂已经被广泛用于治疗炎症性肠病(IBD),但手术仍然是最终的解决方案。75%的患者在其一生中都会经历一次手术治疗。IBD患者经历手术以后全身性炎症反应会明显增加而且术后肠梗阻(POI)的发生率也明显增加。C反应蛋白(CRP)和白介素6(IL-6)水平可以很好反应全身性炎症水平。减少术后过度炎症反应可减少POI并加速术后恢复。因此,这项研究评估了围手术期地塞米松在IBD手术后肠梗阻中的作用。

研究人员对进行手术的IBD患者在麻醉后被随机分配到静脉注射8 mg地塞米松(n = 151)或安慰剂(n = 151)组。主要观察结局是术后肠梗阻延长的发生率。次要结果包括恶心或呕吐发生率,粪便首次通过的时间,术后疼痛,住院时间长和手术并发症等情况。

结果显示:与对照组相比,接受地塞米松治疗的患者术后肠梗阻的发生率较低(22.5%vs 38.4%;P = 0.003),通便时间较短(28 vs 48 h,P <0.001),肠道恢复时间也较短(72 vs 120 h;P <0.001),术后住院时间减少(9.0 vs 10.0 d;P = 0.002),术后疼痛减轻(P <0.05)。但是,术后恶心或呕吐(P = 0.531),术后严重并发症(P = 0.165)或手术部位感染(P>0.5)无显着差异。
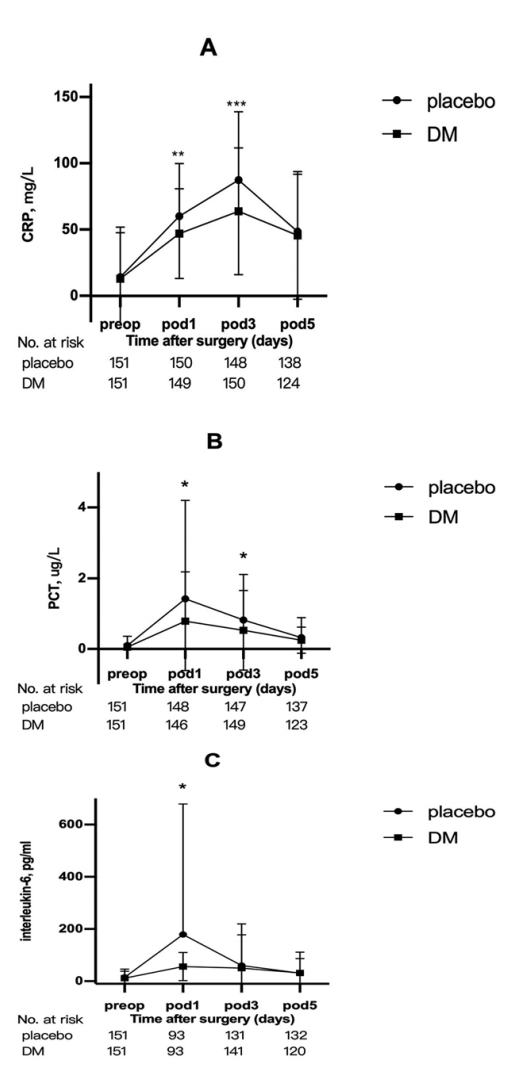
图:炎症指标和术后时间的关系
本项研究证实,单次静脉注射8 mg地塞米松可以降低IBD手术患者的术后肠梗阻的发生率,术后疼痛的强度,并缩短其术后住院时间。
原始出处:
Tenghui Zhang. Et al. Randomized Controlled Trial: Perioperative Dexamethasone Reduces Excessive Postoperative Inflammatory Response and Ileus After Surgery for Inflammatory Bowel Disease. Inflammatory Bowel Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












设计的非常好👍
63
#手术期#
32
感谢分享
61
科研进步,医疗发展!
63
#IBD#
30
#肠梗阻#
33
#炎症反应#
29
好东西
55
666
58
学习让自己更加专业
35