梅斯肿瘤进展速递(第005期)
2021-05-20 Sunny MedSci原创
编者按:梅斯医学将定期进行汇总,帮助大家概览肿瘤领域最新进展。下面是呈现给大家的最近一期的肿瘤进展。enjoy~

编者按:梅斯医学将定期进行汇总,帮助大家概览肿瘤领域最新进展。下面是呈现给大家的最近一期的肿瘤进展。enjoy~
上一期见:梅斯肿瘤进展速递(第004期)
1.J Hematol Oncol:术后循环肿瘤DNA(ctDNA)可用于II/III其结直肠癌患者复发风险预测指标
近日,来自中肿的徐瑞华教授团队联合复旦肿瘤、浙江大学第二医院开展了一项前瞻性、观察性的多中心研究,使用含425基因的NGS检测ctDNA,并且分析其跟II/III期CRC患者复发的关系。其研究成果近期发表在Journal of Hematology & Oncology杂志上。
术后3-7天ctDNA与复发风险关系:所有240例患者进行了术后3-7天的ctDNA检测,20 (8.3%) 例为ctDNA阳性, 而220 (91.7%) 例为ctDNA阴性。ctDNA阴性患者可观察到较低的复发风险, 其2年RFS率为89.4% [95% CI 85.1–93.9%]。相对于ctDNA阴性患者,ctDNA阳性患者的无复发风险则较高(HR=10.98; 95% CI 5.31–22.72; P < 0.001),其2年RFS率为39.3% [95% CI 21.5–71.8%]。5例ctDNA阳性的患者经历了术后辅助化疗后其ctDNA转为阴性。
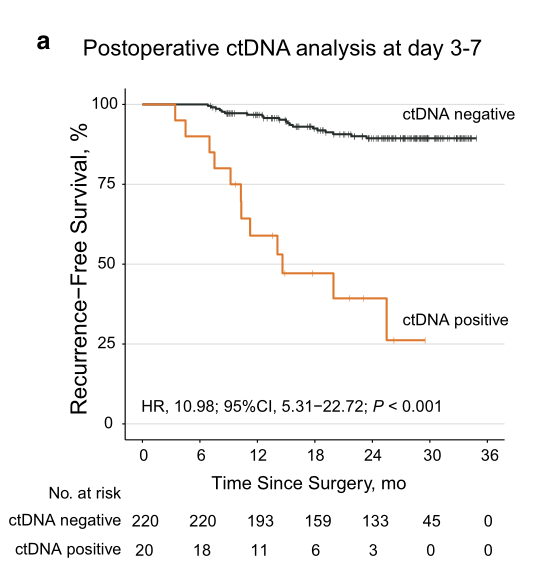
综上,术后连续ctDNA检测可预测II/III CRC患者术后复发的风险以及在影像学诊断前鉴别复发。ctDNA有可能在今后辅助术后患者治疗策略的选择。
详情参考:J Hematol Oncol:术后循环肿瘤DNA(ctDNA)可用于II/III其结直肠癌患者复发风险预测指标
2.Liver Cancer:仑伐替尼(Lenvatinib)治疗晚期肝细胞癌(HCC)失败后的小分子靶向药物治疗的选择
基于目前的临床试验,大都是基于索拉非尼一线治疗,进展后探索二线或以上的治疗方式。但是仑伐替尼一线治疗后进展,二线或以上的治疗很少有探索。而近期,来自日本的研究团队,在Liver Cancer 杂志上发表了一项研究成果,探索一线仑伐替尼治疗晚期HCC患者进展后比较合适的二线治疗方式。
该研究为多中心的回顾性研究,纳入来自日本7个研究中心2018年3月23日至2019年9月30日期间晚期HCC一线接受仑伐替尼治疗的患者。一共178例患者纳入研究,81.5%患者为男性, 中位年龄为73岁(范围:33–95岁), 25.3%患者伴有血管侵犯,36.0% 患者伴有肝外转移。
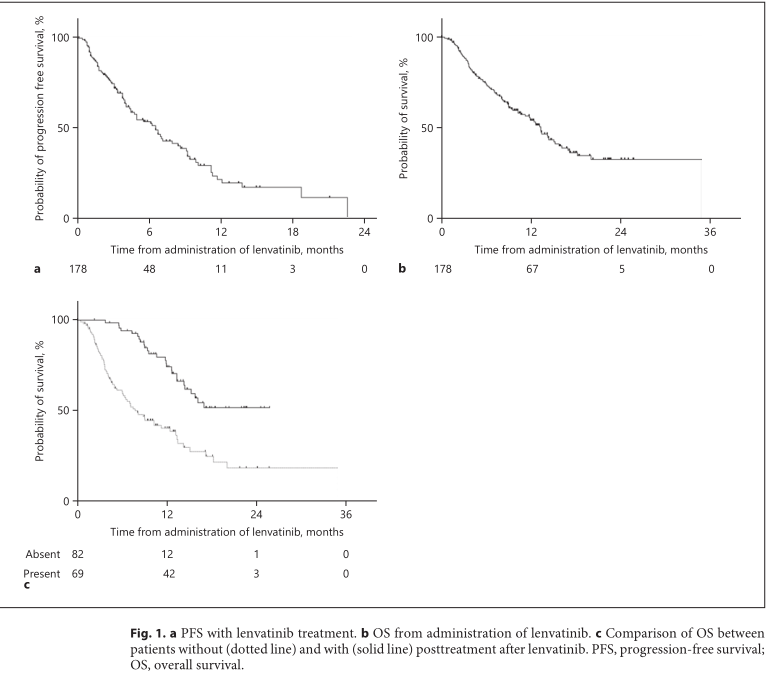 仑伐替尼对生存的影响
仑伐替尼对生存的影响
研究认为,仑伐替尼治疗晚期肝细胞癌(HCC)后的小分子靶向药物选择中,瑞戈非尼可能是比较好的选择。
详情参考:Liver Cancer:仑伐替尼(Lenvatinib)治疗晚期肝细胞癌(HCC)失败后的小分子靶向药物治疗的选择
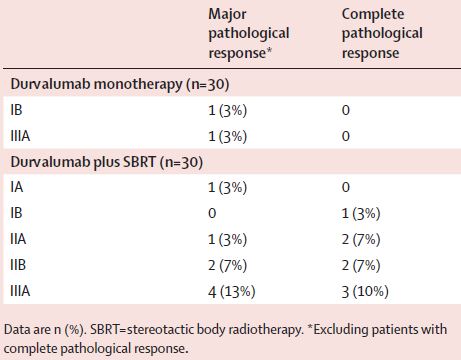
3.Lancet Oncol:杜鲁伐单抗联合立体定向放疗明显改善早期NSCLC患者预后
本研究旨在评估在早期NSCLC患者中使用立体定向放射疗法作为免疫调节剂,以增强与抗PD-L1抗体杜鲁伐单抗相关的抗肿瘤免疫应答的效果。
这是一项单中心、开放标签的、随机对照的2期试验,对比了新辅助杜鲁伐单抗单药治疗和联合立体定向放疗用于早期NSCLC患者的疗效和安全性。招募了可手术切除的早期NSCLC患者,1:1随机分至两组。主要终点是主要病理缓解率。
杜鲁伐单抗单药组有两位患者获得了主要病理缓解(6.7%,95%CI 0.8-22.1),而联合组有16位患者获得了主要病理缓解(53.3%,95%CI 3.2-79.6;p<0.0001)。两组之间的主要病理缓解率差异显着(粗略优势比 16.0, 95% CI 3.2–79.6; p<0.0001)。在联合组获得主要病理缓解的16位患者中,有8位(50%)为完全病理缓解。
主要和完全病理缓解情况
联合组有3位(10%)患者因免疫相关不良事件撤销了第二疗程的杜鲁伐单抗。杜鲁伐单抗单药组有5位(17%)患者发生了3-4级不良反应,联合组有6位(20%)。
综上所述,杜鲁伐单抗新辅助治疗联合立体定向放疗的耐受性良好,安全性高,且可提高早期NSCLC患者的主要病理缓解率。应开展更大规模的试验验证该治疗策略。
详情参考:Lancet Oncol:杜鲁伐单抗联合立体定向放疗明显改善早期NSCLC患者预后
4.JCO:早期定量PET-CT检查或可预测乳腺癌靶向治疗的反应性
共招募了88位患者,其中83位可评估。85%(75/88)的患者完成了4个疗程的RT治疗。单纯RT治疗后的病理完全缓解率为22%。C1D15时对SULmax的百分比变化进行特征分析,得到曲线下的面积 0.72(80%CI 0.64-0.80;单边p=0.12),未拒绝无效假设。
A:C1D15时的SULmax变化;B:有无pCR患者的SULmax变化
但是,获得pCR和未获得pCR的患者相比,SULmax的中位下降百分比有显著差异(63.8% vs 41.8%;p=0.004),SULmax降低≥40%的比例差异更明显(83% vs 52%;p=0.03;阳性预测值 31%)。
C1D15时,SULmax降低不超过40%的患者不太可能获得病理完全缓解(阴性预测值 91%)。
综上,虽然主要目的未达到,但研究结果提示,SULmax的早期变化可预测ER阴性、HER2阳性乳腺癌患者对PT治疗的反应。未来这种定量成像策略可能有助于优化患者的治疗方案。
详情参考:JCO:早期定量PET-CT检查或可预测乳腺癌靶向治疗的反应性
5.Liver Cancer:肝细胞癌伴有血管侵犯的患者手术切除和系统性治疗的疗效比较
来自美国的团队在Liver Cancer杂志上发表了一项研究结果,评估HCC患者伴有血管侵犯手术切除和系统治疗的疗效,以及跟手术切除相关的因素。
多因素分析表明,女性患者的生存期(OS)较男性明显延长(调整的HR(AHR)=0.873, 95% CI: 0.793–0.962);另外, AFP升高(AHR: 1.278, 95% CI: 1.132–1.443) 、更高的MELD评分 (AHR per 10 units: 1.137, 95% CI: 1.084–1.193)和肿瘤大小(AHR: 1.011, 95% CI: 1.007–1.015)是HCC伴有血管侵犯患者的危险因素。
手术切除对OS的影响:30天内再次入院比例和死亡率分别为10.2和8.5%。一线治疗中手术切除对比系统治疗的中位OS为21.4个月和8.1个月(AHR=0.496, 95% CI: 0.426–0.578)。而且,亚组分析表明,非肝硬化患者(AHR=0.550, 95% CI: 0.326–0.926)以及肝硬化患者(AHR: 0.460, 95% CI: 0.311–0.679)中手术切除均较系统治疗明显延长患者的OS。
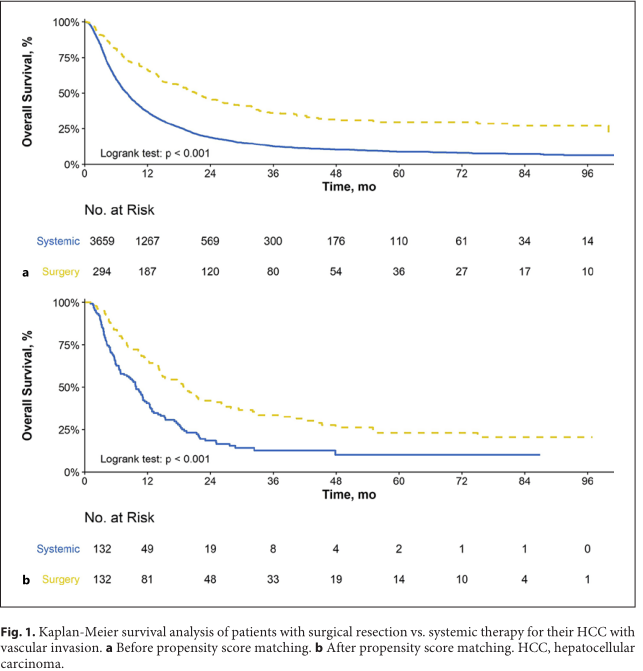 手术切除和系统治疗对生存影响
手术切除和系统治疗对生存影响
研究认为,HCC患者伴有血管侵犯,接受手术切除较系统治疗能够延长患者的OS。
详情参考:Liver Cancer:肝细胞癌伴有血管侵犯的患者手术切除和系统性治疗的疗效比较
6.JAMA:USPSTF结直肠癌筛查最终建议:起始年龄从50岁更新为45岁
5月18日,美国预防医学工作组(USPSTF)建议和大量证据在JAMA在线发表。
CRC的风险因素
正如USPSTF作者指出的,年龄是CRC最重要的风险因素之一,近94%的CRC新发病例发生在45岁及以上的成年人中。CRC筛查开始年龄降低的证据基于模拟模型,表明45岁开始筛查与50岁开始筛查相比,预计与额外增加22至27生命年有关。
USPSTF继续建议对所有50至75岁的成年人进行CRC筛查,将筛查年龄降低到45岁确认了以下事实:在2020年,11%的结肠癌和15%的直肠癌发生在50岁以下的患者中。
与先前2016年发布的指南类似,更新后的USPSTF建议继续提供筛查策略菜单,尽管每个筛查策略的筛查频率各不相同。推荐的筛查策略包括:
·高灵敏度愈创木脂粪便隐血检测或粪便免疫化学检测(FIT) 每年一次
·粪便DNA-FIT检测 每1到3年一次
·CT结肠成像检查 每5年一次
·软式乙状结肠镜检查 每5年一次
·软式乙状结肠镜检查 每10年一次 加上FIT每年一次
·结肠镜筛查 每10年一次
详情参考:JAMA:USPSTF结直肠癌筛查最终建议:起始年龄从50岁更新为45岁
7.AJOG:晚期子宫内膜癌是否有必要进行肿瘤细胞减灭术?
本研究旨在总结肿瘤细胞减灭术(PCS)治疗晚期子宫内膜癌的效果。
Albright等人采用检索词“子宫内膜癌”、“晚期”和“肿瘤细胞减灭术”检索了MEDLINE、Embase和Scopus数据库从创建到2020年9月11日期间包含≥10例接受PCS治疗的晚期子宫内膜癌患者、并有根据PCS后残留肿瘤程度报告发病率和生存结果的全英文文献。两个审稿人独立筛选研究,并由第三个审稿人审核。
共筛查了1219项研究,最终纳入了其中34项研究,包含单中心和多中心研究、跨越6-24年、各种病理类型(子宫内膜样/浆液性/透明细胞/癌肉瘤)和分期(III/IV期)。
在IV期与III-IV期疾病的研究中,肿瘤细胞减少到上述两个阈值的比例都较低(NGRD:41.4% vs 69.8%;<1 cm:63.2% vs 82.2%),但没有明显的组织学差异。
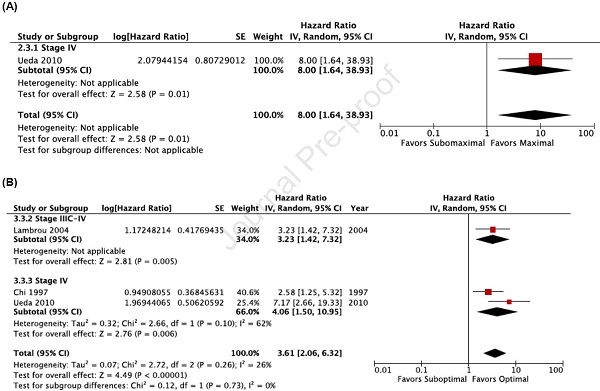
在针对报告的危险比(HR)进行分析时,与NGRD相比,任何可见残留病灶与较差的无进展生存期和总生存期相关(HR分别是2.16, 95%CI 1.45-3.21;I2=68%和2.57, 95%CI 2.13-3.10;I2=1%);与残留病灶<1cm相比,残留病灶≥1cm与较差的无进展生存期和总生存期相关(HR分别是2.55, 95%CI 1.93-3.37;I2=63%和2.62, 95%CI 2.20-3.11;I2=15%)。仅限于高质量研究的敏感性分析结果一致。
总而言之,一定比例的接受PCS治疗的晚期子宫内膜癌患者有残留的肿瘤病灶,与较差的生存预后相关;换言之,大部分患者PCS后的残留肿瘤病灶较小(肉眼不可见或<1cm),与相对较好的无进展生存期和总生存期相关。
详情参考:AJOG:晚期子宫内膜癌是否有必要进行肿瘤细胞减灭术?
8.Liver Cancer:肿瘤微环境的神经纤维密度(NFD)是肝门部胆管癌(pCCA)术后的重要预后指标
来自德国的研究团队在Liver Cancer杂志上发表了相关研究,评估NFD在手术切除后pCCA患者的预后价值。
研究结果,中位随访时间为53个月时,总人群中位CSS为49个月(95% CI: 29–69),中位OS为33个月(95% CI: 19–47),中位PFS为37个月(95% CI: 18–56)。高NFD患者中位CSS为90个月(95% CI: 48–132, 3-year CSS = 77%, 5-year CSS = 72%),而低NFD患者的中位CSS为33个月(95% CI: 19–47, 3-year CSS = 46%, 5-year CSS = 32%),两组CSS有明显的统计学差异(p =0.006)。高NFD患者中位RFS为83个月(95% CI: 34–132),而低NFD患者的中位RFS为24个月(95% CI: 13–35),两组RFS有明显的统计学差异(p =0.004)。
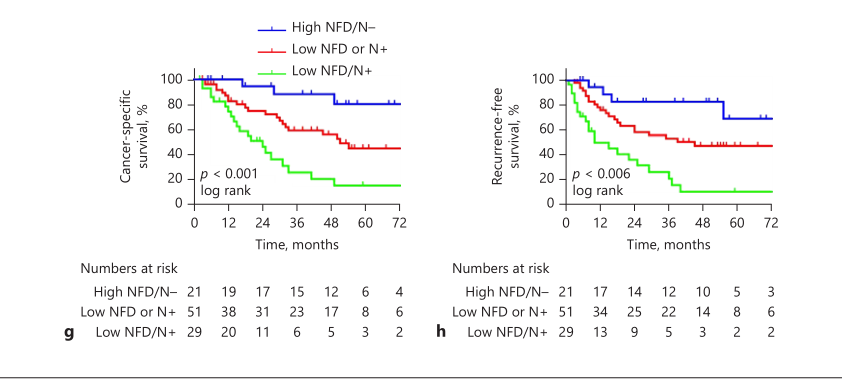 NFD联合淋巴结对CSS和RFS的影响
NFD联合淋巴结对CSS和RFS的影响
研究认为,神经纤维密度(NFD)是肝门部胆管癌(pCCA)重要的预后指标,其单独或与淋巴结联合可很好的预测术后pCCA患者的临床预后。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#肿瘤进展#
41
好文章
65
#梅斯#
36
很好的进展
73
#肿瘤#好内容!!
93
好文章
73
好文章!
75