Eur Urol:中、高风险前列腺癌根治性前列腺切除术中盆腔淋巴结切清扫的扩大与限制比较
2020-12-22 AlexYang MedSci原创
扩大盆腔淋巴结切除术(EPLND)在前列腺癌(PCa)患者手术治疗中的作用仍存在争议,主要是因为缺乏随机对照试验(RCTs)。最近,有研究人员确定了是否EPLND与有限制的PLND(LPLND)有更好
扩大盆腔淋巴结切除术(EPLND)在前列腺癌(PCa)患者手术治疗中的作用仍存在争议,主要是因为缺乏随机对照试验(RCTs)。最近,有研究人员确定了是否EPLND与有限制的PLND(LPLND)有更好的肿瘤学结果。

研究时一项前瞻性、单中心的3期试验,研究对象为中风险或高风险临床局部PCa患者。研究共有300名随机来自2012年5月到2016年12月的患者(150名LPLND和150名EPLND)。LPLND组的五生化复发生存(BRFS)中位数为61.4个月,EPLND组未达到(HR 0.91,95%CI 0.63-1.32;p=0.6)。两组均未达到中位无转移生存(MFS)(HR 0.57,95%CI 0.17-1.8;p=0.3)。由于没有患者在截止日期前死于PCa,因此无法获得癌症特异性生存(CSS)数据。在探索性亚组分析中,被分配到EPLND的术前活检国际泌尿系统病理学会(ISUP)3-5级组的患者具有更好的BRFS(HR 0.33,95%CI 0.14-0.74,interaction p=0.007)。另外,较短的随访时间和外科医生的异质性是本研究的局限性。
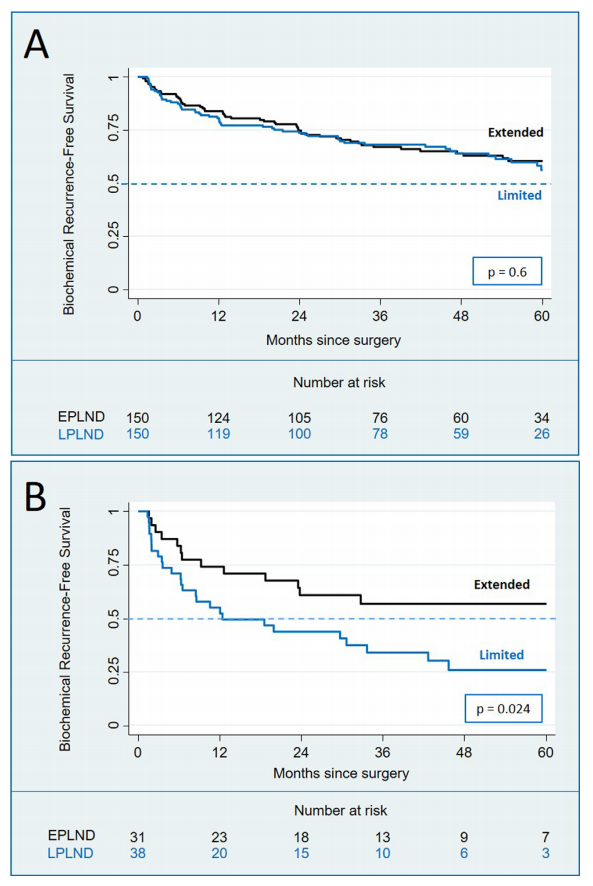
最后,研究人员指出,他们的RCT证实了EPLND提供了更好的病理分期,而并未揭示早期肿瘤学结果的差异。他们的亚组分析表明,在诊断为ISUP 3-5级组的患者中具有潜在的BCRFS益处;然而,这些研究结果有必要进行更大队列和更长随访时间的RCT来更好的确定EPLND在RP中的作用。
原始出处:
Jean F P Lestingi, Giuliano B Guglielmetti, Quoc-Dien Trinh et al. Extended Versus Limited Pelvic Lymph Node Dissection During Radical Prostatectomy for Intermediate- and High-risk Prostate Cancer: Early Oncological Outcomes from a Randomized Phase 3 Trial. Eur Urol. Dec 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#高风险#
38
#切除术#
27
#前列腺切除#
30
学习了
66
#淋巴结#
36
#根治#
27
前列腺癌相关研究,学习了,谢谢梅斯
0